2. Tetreault LA, Karadimas S, Wilson JR, Arnold PM, Kurpad S, Dettori JR, et al. The natural history of degenerative cervical myelopathy and the rate of hospitalization following spinal cord injury: an updated systematic review. Global Spine J 2017;7(3 Suppl):28S-34S.

4. Schöps TF, Schneider MP, Steffen F, Ineichen BV, Mehnert U, Kessler TM. Neurogenic lower urinary tract dysfunction (NLUTD) in patients with spinal cord injury: long-term urodynamic findings. BJU Int 2015;115 Suppl 6:33-8. PMID:
25891318 

5. Andy UU, Harvie HS, Smith AL, Propert KJ, Bogner HR, Arya LA. Validation of a self-administered instrument to measure adherence to anticholinergic drugs in women with overactive bladder. Neurourol Urodyn 2015;34:424-8. PMID:
24719232 

8. Yan HL, Zong HT, Cui YS, Li N, Zhang Y. Calcineurin inhibitor avoidance and withdrawal for kidney transplantation: a systematic review and meta-analysis of randomized controlled trials. Transplant Proc 2014;46:1302-13. PMID:
24935293 

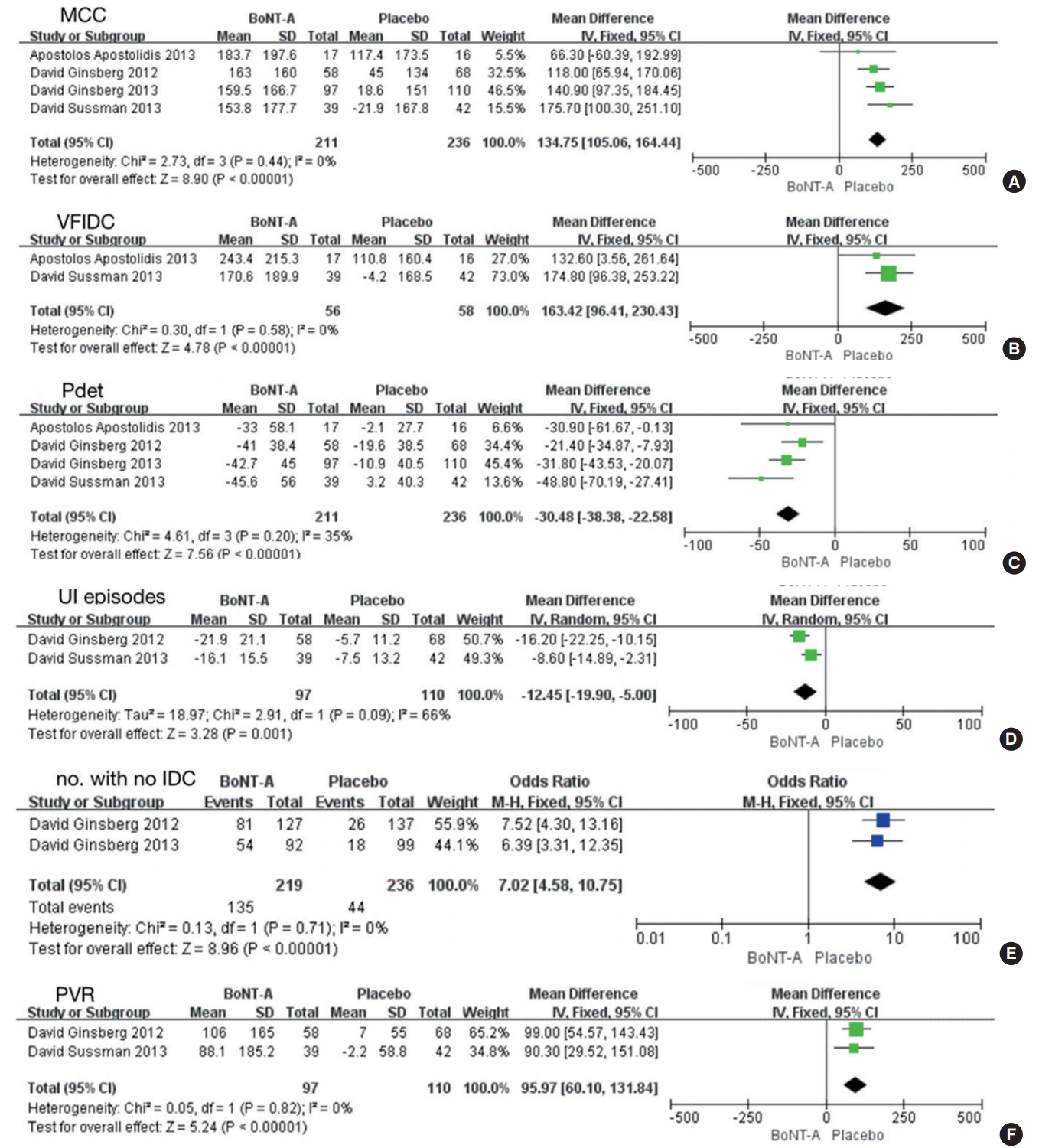
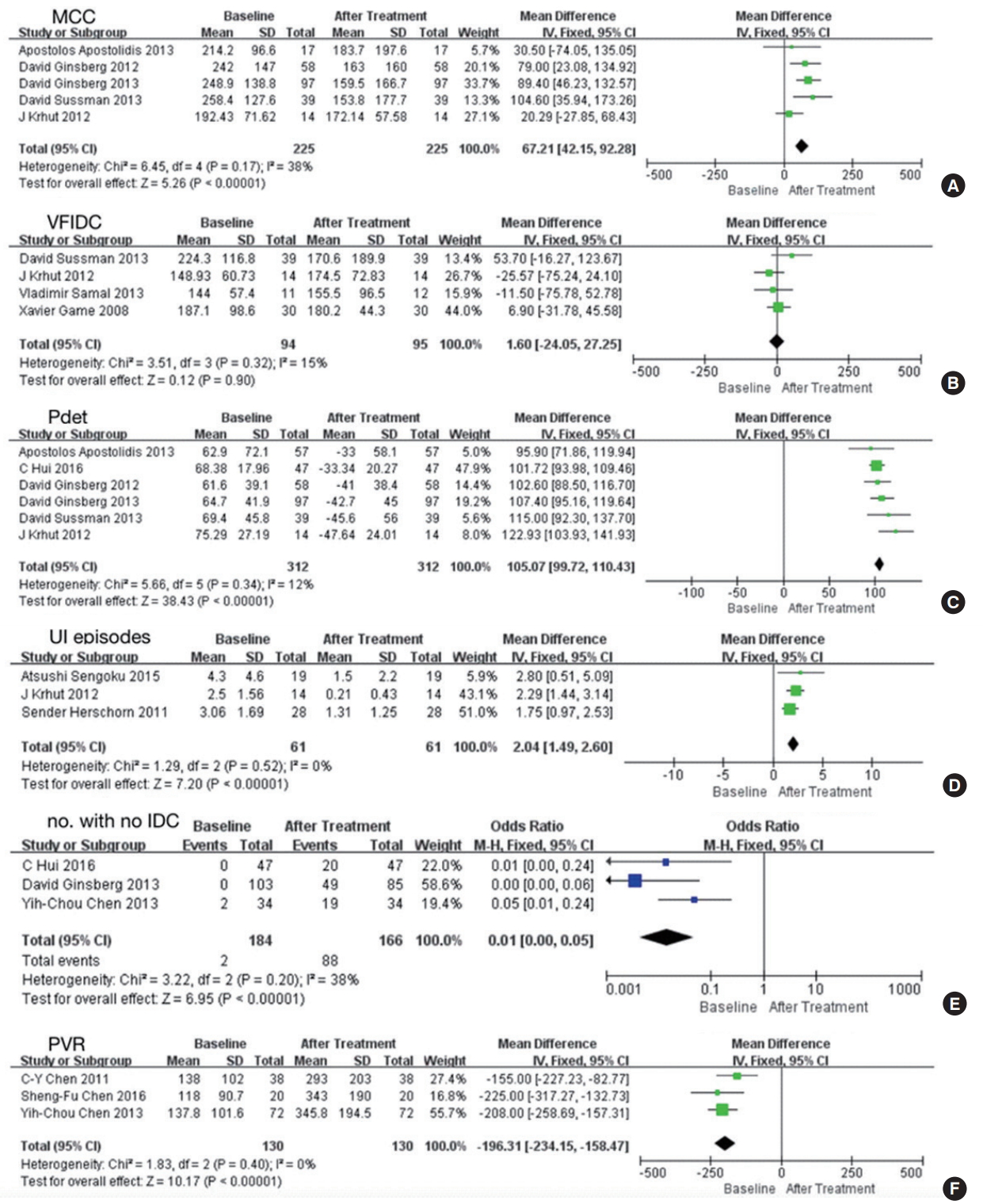
11. Apostolidis A, Thompson C, Yan X, Mourad S. An exploratory, placebo-controlled, dose-response study of the efficacy and safety of onabotulinumtoxinA in spinal cord injury patients with urinary incontinence due to neurogenic detrusor overactivity. World J Urol 2013;31:1469-74. PMID:
23160758 

12. Sussman D, Patel V, Del Popolo G, Lam W, Globe D, Pommerville P. Treatment satisfaction and improvement in health-related quality of life with onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity. Neurourol Urodyn 2013;32:242-9. PMID:
22965657 

13. Cruz F, Herschorn S, Aliotta P, Brin M, Thompson C, Lam W, et al. Efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: a randomised, double-blind, placebo-controlled trial. Eur Urol 2011;60:742-50. PMID:
21798658 

14. Ginsberg D, Gousse A, Keppenne V, Sievert KD, Thompson C, Lam W, et al. Phase 3 efficacy and tolerability study of onabotulinumtoxinA for urinary incontinence from neurogenic detrusor overactivity. J Urol 2012;187:2131-9. PMID:
22503020 

15. Chen SF, Chang CH, Kuo HC. Clinical efficacy and changes of urothelial dysfunction after repeated detrusor botulinum toxin A injections in chronic spinal cord-injured bladder. Toxins (Basel) 2016 May 30;8(6):pii: E164.
https://doi.org/10.3390/toxins8060164.

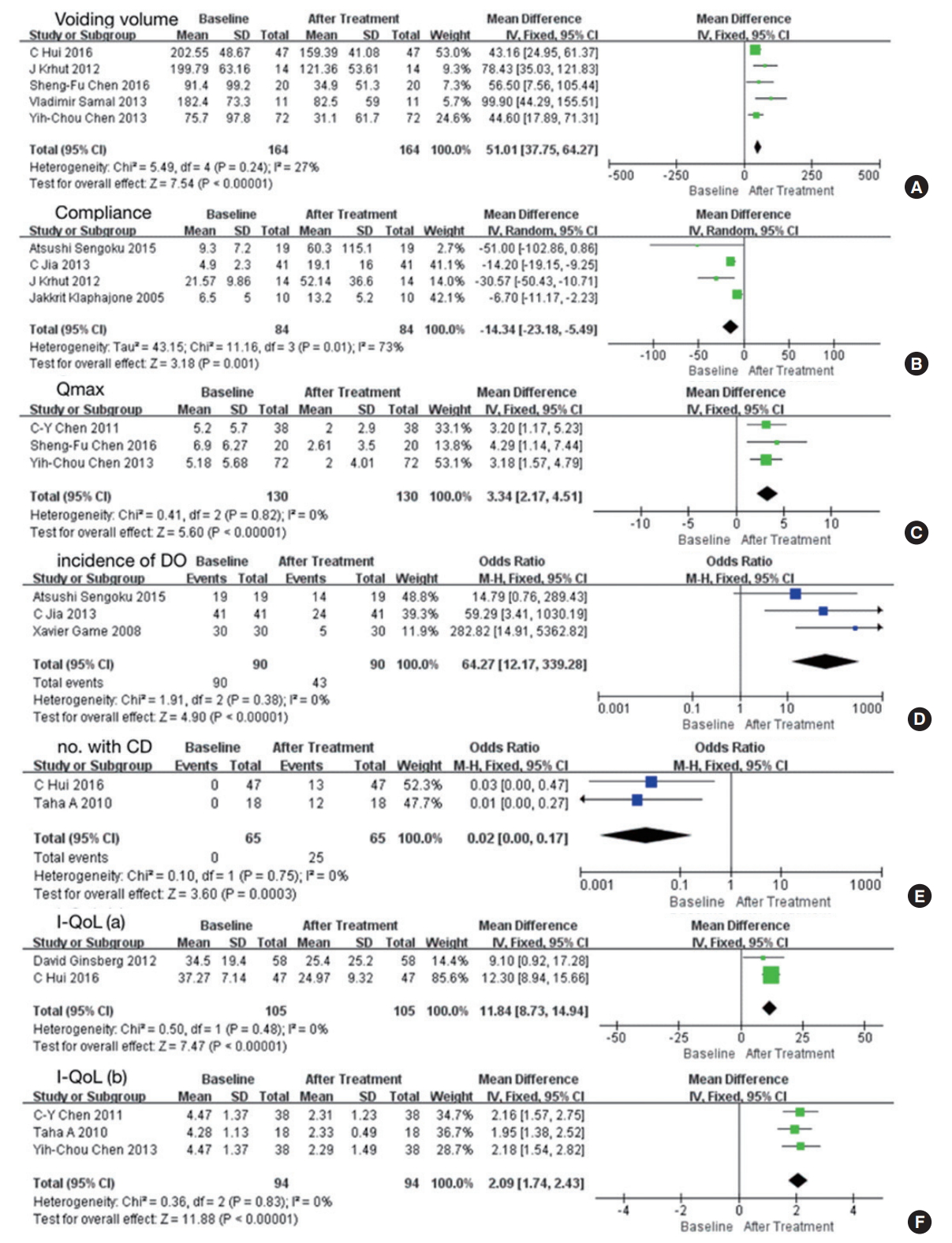
17. Sengoku A, Okamura K, Kimoto Y, Ogawa T, Namima T, Yamanishi T, et al. Botulinum toxin A injection for the treatment of neurogenic detrusor overactivity secondary to spinal cord injury: multiinstitutional experience in Japan. Int J Urol 2015;22:306-9. PMID:
25403926 

18. Chen YC, Kuo HC. The therapeutic effects of repeated detrusor injections between 200 or 300 units of onabotulinumtoxinA in chronic spinal cord injured patients. Neurourol Urodyn 2014;33:129-34. PMID:
23494629 

21. Gamé X, Castel-Lacanal E, Bentaleb Y, Thiry-Escudié I, De Boissezon X, Malavaud B, et al. Botulinum toxin A detrusor injections in patients with neurogenic detrusor overactivity significantly decrease the incidence of symptomatic urinary tract infections. Eur Urol 2008;53:613-8. PMID:
17804150 

22. Klaphajone J, Kitisomprayoonkul W, Sriplakit S. Botulinum toxin type A injections for treating neurogenic detrusor overactivity combined with low-compliance bladder in patients with spinal cord lesions. Arch Phys Med Rehabil 2005;86:2114-8. PMID:
16271557 

23. Abdel-Meguid TA. Botulinum toxin-A injections into neurogenic overactive bladder--to include or exclude the trigone? A prospective, randomized, controlled trial. J Urol 2010;184:2423-8. PMID:
20952003 

24. Šámal V, Mečl J, Šrám J. Submucosal administration of onabotulinumtoxinA in the treatment of neurogenic detrusor overactivity: pilot single-centre experience and comparison with standard injection into the detrusor. Urol Int 2013;91:423-8. PMID:
23774308 

25. Herschorn S, Gajewski J, Ethans K, Corcos J, Carlson K, Bailly G, et al. Efficacy of botulinum toxin A injection for neurogenic detrusor overactivity and urinary incontinence: a randomized, double-blind trial. J Urol 2011;185:2229-35. PMID:
21497851 

26. Schurch B, Denys P, Kozma CM, Reese PR, Slaton T, Barron RL. Botulinum toxin A improves the quality of life of patients with neurogenic urinary incontinence. Eur Urol 2007;52:850-8. PMID:
17467889 

27. Schurch B, Denys P, Kozma CM, Reese PR, Slaton T, Barron R. Reliability and validity of the Incontinence Quality of Life questionnaire in patients with neurogenic urinary incontinence. Arch Phys Med Rehabil 2007;88:646-52. PMID:
17466735 

28. Schurch B, de Sèze M, Denys P, Chartier-Kastler E, Haab F, Everaert K, et al. Botulinum toxin type a is a safe and effective treatment for neurogenic urinary incontinence: results of a single treatment, randomized, placebo controlled 6-month study. J Urol 2005;174:196-200. PMID:
15947626 

29. Zakin E, Simpson D. Evidence on botulinum toxin in selected disorders. Toxicon 2018;147:134-40. PMID:
29408357 

30. Smith CP, Boone TB, de Groat WC, Chancellor MB, Somogyi GT. Effect of stimulation intensity and botulinum toxin isoform on rat bladder strip contractions. Brain Res Bull 2003;61:165-71. PMID:
12832003 

31. Nuanthaisong U, Abraham N, Goldman HB. Incidence of adverse events after high doses of onabotulinumtoxinA for multiple indications. Urology 2014;84:1044-8. PMID:
25443898 

32. Khera M, Somogyi GT, Kiss S, Boone TB, Smith CP. Botulinum toxin A inhibits ATP release from bladder urothelium after chronic spinal cord injury. Neurochem Int 2004;45:987-93. PMID:
15337297 

33. Do TP, Hvedstrup J, Schytz HW. Botulinum toxin: A review of the mode of action in migraine. Acta Neurol Scand 2018;137:442-51. PMID:
29405250