Nocturia Improvement With Surgical Correction of Sleep Apnea
Article information
Abstract
Purpose
To evaluate changes in nocturia after surgical correction of obstructive sleep apnea (OSA).
Methods
A total of 66 patients were included in the present study. All had been diagnosed with OSA syndrome by polysomnography and underwent uvulopalatopharyngoplasty (UPPP). Preoperative and postoperative lower urinary tract symptoms (LUTS), quality of life (QoL), and nocturia episodes were evaluated using the International Prostate Symptom Score (IPSS) and overactive bladder symptom score (OABSS) questionnaires. Three months postoperatively, telephone interviews were performed to determine the success of surgery, current LUTS, and nocturia episodes. Patients were divided into surgical success and failure groups. Surgical success was defined as snoring decrease more than 50% based on the patient’s subjective judgment.
Results
The response rate was 56% and success rate was 73%. In all patients, nocturia episodes significantly decreased from 1.7±1.1 to 0.8±1.2 (P=0.002). Mean IPSS score, OABSS score, and QoL scores were also significantly improved. The success group showed a significant decrease in nocturia episodes, and total IPSS, OABSS, and QoL scores. However, the failure group did not show significant changes in all parameters.
Conclusions
OSA correction improved nocturia as well as other LUTS. These improvements were not observed in the failure group. This study shows that OSA is a cause of nocturia and that other LUTS and nocturia can be improved by surgical correction of OSA.
INTRODUCTION
Nocturia is common lower urinary tract symptoms (LUTS). The Boston Area Community Health study showed that nocturia affected 25% of men and 31% of women [1]. In the Epidemiology of Urinary Incontinence and Comorbidities study, the prevalence of nocturia was 49% in men and 55% in women [2].
Nocturia is not only a common voiding problem but also reduces the quality of life (QoL) and is associated with sleep disruption and daytime fatigue [3,4]. Nocturia is also reported to be associated with a twofold increase in the risk of falls in a 24-hour day [5].
Therefore, nocturia is an important concern for physicians who treat LUTS patients, but is not easily treatable. Except in the case of nocturnal polyuria, nocturia has usually been managed as an isolated symptom, with therapy based on LUTS, including alpha blockers and anticholinergic drugs. Recent research suggests, however, that the etiology of nocturia differs from that of other LUTS, and that nocturia should be evaluated as a separate condition, as well as a component of a systemic disease [6].
Among systemic diseases, obstructive sleep apnea (OSA) syndrome has shown an association with nocturia in several studies. Oztura et al. [7] reported that the prevalence of nocturia increased with an increase in OSA severity. Community-based elderly populations with higher rates of sleep-disordered breathing ( >25 breathing events/hr) have nearly double the number of nocturia episodes, compared with those with low rates of OSA [8].
Therefore, the correction of OSA would be expected to reduce the severity of nocturia. One study showed that continuous positive airway pressure (CPAP) treatment of OSA significantly reduced the frequency of nocturia [9]. However, to our knowledge, there is no report on nocturia improvement with surgical correction of sleep apnea.
Although CPAP is recommended for primary treatment of OSA, its effectiveness is often limited by poor compliance and acceptance [10]. Furthermore, CPAP treatment has several adverse effects including nasal obstruction, mask leak, skin breakdown, pressure intolerance, and claustrophobia [11,12]. Therefore, some patients select surgical therapy [13]. Among numerous OSA surgical procedures according to the obstructive level, uvulopalatopharyngoplasty (UPPP) is one of the most popular for treating oropharyngeal obstruction [14].
In this study, we evaluated changes in nocturia episodes after UPPP, to determine whether nocturia is decreased after correction of OSA. We also investigated the effect of surgical treatment on other LUTS and related QoL.
MATERIALS AND METHODS
Study Subjects
Between 2012 and 2014, 256 patients who consulted for a sleep problem were diagnosed with OSA by polysomnography. Of these, 66 who planned to undergo UPPP surgery for correction of OSA were included in this study. Subjects eligible for UPPP surgery were adults (age ≥18 years) who (1) complained of clinical symptoms suggestive of OSA without nasal obstruction; (2) had an apnea-hypopnea index (AHI) ≥5 per hour of total sleep time on diagnostic polysomnography; and (3) refused medical treatment such as CPAP or an oral appliance.
Study inclusion criteria were clinically proven OSA, nocturia episodes ≥1, age >20, and planning to undergo UPPP. Exclusion criteria were a history of taking medication for LUTS caused by benign prostatic hyperplasia (BPH), overactive bladder (OAB), or other etiologies. All patients provided informed consent, and the study protocol was approved by the ethics committee of Konkuk University Hospital (approval number: KUH1130050).
The primary endpoint of the study was a change in nocturia episodes. The secondary endpoints were changes in International Prostate Symptom Score (IPSS), QoL score, and overactive bladder symptom score (OABSS) at 3 months after surgery. Pre- and postoperative IPSS, QoL score, and number of nocturia episodes were evaluated using the IPSS and OABSS questionnaires.
Polysomnography
Nocturnal polysomnography was performed using an Embla N7000 system (Medcare-Embla, Reykjavik, Iceland) and Somnologica ver. 3.3.1 software (Medcare-Embla) when subjects were in bed from lights-off to lights-on. Electroencephalography was monitored using C3/A2 and C4/A1, and O1/A2 and O2/A1 lead pairs. Two pairs of electrooculography leads were used. Electromyographic leads were placed on the submentalis and tibialis anterior muscles. Airflow was continuously measured by a thermistor and nasal pressure cannula. Respiratory movements were monitored using inductive plethysmography belts around the chest and abdomen. Oxygen saturation was measured by a pulse oximeter sensor on the left second finger. Apnea was defined as an 80% or greater reduction in airflow for at least 10 seconds.
UPPP
All UPPPs were performed under general anesthesia by 2 surgeons. Tonsils were removed and redundant posterior pillar tissue was trimmed. The anterior and posterior pillars were then sutured to each other. The uvula was preserved as much as possible.
Postoperative Evaluation
At 3 month after surgery, telephone interviews were performed to determine surgical success, current LUTS, and status of nocturia episodes.
Surgical success was defined as snoring decrease more than 50% based on the patient’s subjective judgment, and patients were divided into success and failure groups.
The number of nocturia episodes was evaluated by IPSS questionnaire item 7: “Over the past month, how many times per night did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning?” QoL was estimated by the IPSS QoL item. Postoperative OAB symptoms were evaluated using the OABSS questionnaire.
Statistical Analysis
Pre- and postoperative nocturia episodes, total IPSS, QoL score, and OABSS were compared in all patients; the success group was evaluated with the paired t-test and the failure group by the Wilcoxon signed rank test. Statistical analyses were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA), and P-values of <0.05 were considered significant.
RESULTS
Of 66 patients, 37 (mean age: 45.0±12.3 years) responded to telephone interviews. The response rate was 56% and the UPPP success rate was 73%. The characteristics of the patients are described in Table 1.
Overall Results
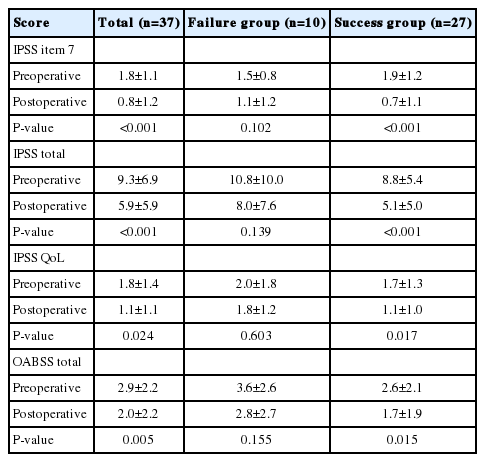
Overall, voiding and storage parameters including nocturia were improved after OSA correction surgery (Table 2). Nocturia episodes were significantly decreased from 1.8±1.1 to 0.8±1.2 (P<0.001). Total mean IPSS was decreased from 9.3±6.9 to 5.9±5.9 (P<0.001) and OABSS was decreased from 2.9±2.2 to 2.0±2.2 (P=0.005). QoL score decreased from 1.8±1.4 to 1.1±1.1 (P=0.02) (Fig. 1).
Changes in lower urinary tract symptoms following uvulopalatopharyngoplasty in all patients. (A) Change of IPSS item 7 (nocturia) score, (B) change of total IPSS score, (C) change of IPSS QoL score, amd (D) change of total OABSS score. IPSS, International Prostate Symptom Score; QoL, quality of life; OABSS, overactive bladder symptom score. *P<0.05.
Success Group and Failure Group
Age and preoperative AHI were similar between the success (n=27) and failure groups (n=10). There were no differences in preoperative nocturia episodes, total IPSS score, and OABSS score between the 2 groups (Table 2).
After surgery, the success group showed a significant decrease in nocturia episodes (from 1.9 to 0.7, P<0.001). In 15 patients (41%), the nocturia episodes decreased to zero. Total IPSS score (from 8.8 to 5.1, P<0.001), OABSS score (2.6 to 1.7, P=0.015), and QoL score (from 1.7 to 1.1, P=0.017) were all significantly decreased. However, the failure group did not show a significant change in nocturia episodes or other parameters (Fig. 2).
Changes in lower urinary tract symptoms following uvulopalatopharyngoplasty by group. (A) Change of IPSS item 7 (nocturia) score, (B) change of total IPSS score, (C) change of IPSS Qol score, and (D) change of total OABSS score. IPSS, International Prostate Symptom Score; Qol, quality of life; OABSS, overactive bladder symptom score. *P<0.05.
DISCUSSION
Nocturia is a multifactorial condition with many possible urinary causes including BPH and OAB, or nonurinary causes such as diabetes, insomnia, or congestive heart failure. Among the nonurological causes, sleep disturbance due to OSA syndrome is reportedly associated with nocturia. Therefore, the correction of OSA should reduce nocturia episodes.
However, there are few studies showing a decrease in nocturia after treatment of OSA, and only a few studies showed significant improvement in nocturia episodes with nasal CPAP treatment for OSA. Margel et al. [9] reported that nocturia episodes decreased from 2.5 before CPAP to 0.7 after treatment, and Fitzgerald et al. [15] also reported that nocturia decreased significantly in 46 men with OSA treated with CPAP, from a median of 3 to a median of 0 episodes. In 29 patients (60%), the rate of nocturia episodes per hour decreased to zero.
To our knowledge, no study has reported the effect of OSA surgical correction on improvement in nocturia and LUTS. This study showed that surgical correction of OSA improved nocturia episodes and other LUTS. This effect was more definite in the surgical success group. The success group showed a mean 1.2 decrease in nocturia episodes. This result suggested that surgical management of OSA could improve nocturia.
The mechanism of this improvement is not clear. Umlauf et al. [16] found that both nighttime urine production and atrial natriuretic peptide (ANP) secretion are elevated in subjects with severe OSA. They proposed that the obstructive respiratory events combined with sustained ventilatory effort in OSA generate negative intrathoracic pressure, causing the heart to receive a false signal of volume overload. The hormonal response to this signal is increased ANP secretion and increased urinary production. According to this theory, the correction of OSA may eliminate negative intrathoracic pressure and reduce secretion of ANP, which consequently reduces nocturia.
Another possible mechanism is that obstructive apneic events may induce alpha receptor-mediated vasoconstriction and induce hypertension or various cardiovascular diseases [17]. The increased alpha sympathetic nervous activity in patients with OSA is also responsible for LUTS, including nocturia.
Alpha blockers used in LUTS/BPH have shown effects on nocturia; alpha blockers are thought to reduce residual urine and thereby increase capacity for nocturnal urine storage. One study showed that tamsulosin 0.4 mg was superior to placebo in reducing nocturia [18]. Therefore, suppression of increased alpha adrenergic tone by correction of OSA could be one of the mechanisms of nocturia improvement.
This study showed that LUTS other than nocturia were also improved, and that the QoL score was significantly decreased after surgery. These results suggest that correction of OSA suppresses alpha adrenergic tone in the lower urinary tract and facilitates voiding function. Moreover, the lack of improvement in nocturia and LUTS after surgery in failure patients clarified the effect of OSA suppression on LUTS.
Our study has some limitations. Nocturia was evaluated by IPSS questionnaire rather than with a voiding diary. Therefore, we could not identify patients with nocturnal polyuria and also could not determine the effect of surgery on improvement. Moreover, nocturia was evaluated by patient recall, with the possibility of recall or selection bias, because patients with improved OSA symptoms might respond more positively. As previously noted, the number of study subjects was somewhat small for evaluation of the effect of OSA surgery. Finally, we did not perform urodynamic testing, and thus could not determine whether any patients had pathologic urodynamic features.
However, this was the first study to show that surgical correction of OSA decreased nocturia episodes. To clarify this effect, a large-scale prospective study using a voiding diary would be needed.
In conclusion, OSA correction improved LUTS, QoL, and nocturia episodes. Nocturia as well as other LUTS were decreased predominantly in the OSA surgery success group. This study shows that OSA is one of the causes of nocturia and that nocturia can be improved by surgical correction of OSA. We recommend that patients with nocturia should be queried about signs and symptoms of snoring and apnea and referred for surgical correction if indicated.
Notes
Grant Support
This work was supported by Konkuk University Medical Center Research Grant 2015.
Research Ethics
All patients provided informed consent, and the study protocol was approved by the ethics committee of Konkuk University Hospital (approval number: KUH1130050).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.