Long-term Outcomes of Tension-free Vaginal Tape Procedure for Treatment of Female Stress Urinary Incontinence with Intrinsic Sphincter Deficiency
Article information
Abstract
Purpose
To assess the long-term outcomes of tension-free vaginal tape (TVT) for stress urinary incontinence (SUI) with intrinsic sphincter deficiency (ISD) and to identify influencing factors for failure in these cases.
Methods
A total of 136 women who underwent TVT procedures with minimum follow-up duration of 3 years were included in the study. Patients were divided into two groups (non-ISD and ISD groups) based on preoperative urodynamic studies. Patient outcomes were assessed from retrospective chart review and telephone research. Cure was defined as the subjective resolution of SUI in any circumstances. Improvement was defined as the subjective improvement of SUI without complete resolution. Failure was defined as the subjective lack of improvement of SUI. Patients in ISD group were subdivided into two subgroups (cure and non-cure groups) and were compared to identify influencing factors for TVT procedure failure.
Results
Eighty-nine patients were in non-ISD group, and 47 in ISD group. The mean follow-up durations were 50.3±9.2 and 49.7±9.7 months, respectively. Subjective cure rate was 75.3% for non-ISD group, and 76.7% for ISD group (P>0.05). Improvement rate was 6.7% for non-ISD group, and 2.1% for ISD group (P>0.05). Satisfaction scores was 3.8±1.2 points in the non-ISD group, and 3.5±1.2 points in ISD group (P>0.05). In ISD subgroups, VLPP was 41.9±12.0 cmH2O for non-cure group, and 50.5±8.6 cmH2O for cure group, and was the only factor that showed significant statistical difference between the two subgroups (P=0.011).
Conclusions
With our long-term results, TVT is an effective treatment even in women with ISD. However, ISD patients with low VLPP should be counseled carefully about TVT outcome.
INTRODUCTION
Stress urinary incontinence (SUI) is a highly prevalent condition that has a significant impact on health related quality of life. Although multiple behavioral and operative treatments exist, mid-urethral slings are becoming the gold standard for correction of SUI in women.
SUI due to intrinsic sphincter deficiency (ISD) is the most clinical challenges in anti-incontinence operation. In ISD, the urethral closure mechanism is considered to function poorly and historically, pubovaginal slings have been the procedure of choice.
Tension-free vaginal tape (TVT) procedure has been shown to be a safe and effective treatment for stress urinary incontinence with high success rate and this procedure had been employed in patients with ISD. The success rates of TVT procedure in these patients were acceptable with success rate of 73 to 82% [1-3]. However, most reports were short term follow-up studies and there is only one simple long-term observation study.
The aim of our study was to compare the long-term clinical outcomes of the TVT procedure in ISD and non-ISD patients and identify the influencing factors for TVT procedure failure in patients with ISD.
MATERIALS AND METHODS
We retrospectively assessed patients who were urodynamically diagnosed as stress urinary incontinence and those who underwent TVT procedure between 2005 and July 2008. A total of 136 patients with minimum follow-up duration of 3 years were included in the study. All the TVT procedures were performed by one experienced surgeon.
ISD was defined by a maximum urethral closure pressure (MUCP) less than 20 cmH2O or a Valsalva leak point pressure (VLPP) less than 60 cmH2O [4]. Patients were divided into two groups, the non-ISD group and the ISD group. Demographics, urodynamic study, urethral hypermobility, and surgical variables were compared between the two groups. Urethral hypermobility was defined by a straining Q-tip angle greater than 30 degrees from the horizontal [5].
Patient outcomes were assessed from the questionnaires by the retrospective chart review or/and telephone research. Satisfaction scores were assessed by a 5-point Likert-type scale as 1 (completely dissatisfied), 2 (mostly dissatisfied), 3 (neutral), 4 (mostly satisfied), or 5 (completely satisfied). Cure was defined as no urine leakage at all in any circumstances, and improvement was defined as having some urine leakage but over 4 points out of 5 in the satisfaction inquiry. Failure was defined as having some urine leakage and at most 3 points or less out of 5 in the satisfaction inquiry.
Cure rate, improvement rate, failure rate, and satisfaction score after TVT failure were compared between the two groups.
Patients in ISD group were subdivided again into two subgroups, the cure group and non-cure group. Demographics, urodynamic studies, and surgical variables were compared between the two subgroups to identify prognostic factors for TVT failure.
Student's t-test and chi-square test were applied. Reported P-values were 2-sided and a P-value of less than 0.05 was considered statistically significant for all comparisons. Statistical analysis was performed with commercial statistical software SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Demographic variables were comparable between the non-ISD group (n=89) and the ISD group (n=47) (Table 1). Mean age, follow-up duration, body mass index, concomitant cystocele repair and previous operation history also showed no significant differences between the two groups. However, the prevalence of concomitant medical diseases, such as diabetes, hypertension, and cerebrovascular disease was higher in the ISD group.
MUCP and VLPP in the non-ISD group were 79.5±46.9 and 78.7±14.5 cmH2O, and in the ISD group, they were 57.3±28.3 and 48.4±10.0 cmH2O (P<0.05). Maximum urinary flow rate (Qmax), post voided residual urine (PVR), and urethral hypermobility rate were not significantly different between the two groups (Table 1).
The cure rate of TVT showed no difference between the two groups. Sixty-seven (75.3%) of 89 patients were cured in non-ISD group and 36 of 47 patients (76.6%) were cured in ISD group. Satisfaction scores in the non-ISD and ISD groups were 3.8±1.2 points and 3.5±1.2 points, respectively and were not different between the two groups (Table 2).
In non-ISD group, 2 patients had vaginal erosion and 1 patient had urinary tract infection during follow-up duration. In ISD group, no patient had any kind of erosion and 1 patient had urinary retention.
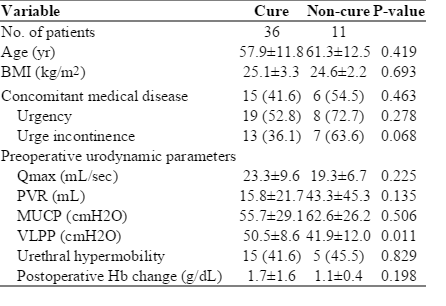
ISD group was subdivided into cure group (n=36) and non-cure group (n=11). Age, concomitant medical disease, concomitant overactive bladder symptoms, MUCP and urethral hypermobility were not statistically different between the two subgroups. The only significant parameter was the VLPP. VLPP of the cure and non-cure subgroups were 41.9±12.0 cmH2O and 50.5±8.6 cmH2O, which was statistically significant (P=0.011) (Table 3).
DISCUSSION
The TVT procedure has become one of the most popular techniques for treating SUI because of its ease and effectiveness. A published series [6,7] with a long follow-up duration showed good continence rates after the TVT procedure.
However, there is a controversy about the long term efficacy of the TVT procedure in women with ISD. Doo et al. [8] reported five year follow-up results 31 patients with VLPP below 60 cmH2O and 64 with VLPP above 60 cmH2O. Cure rates were 51.6% and 82.8%, respectively and the success rate of the ISD group was significantly lower. Paick et al. [2] also reported significantly low success rate in the group below 60 cmH2O compared the group above 60 cmH2O.
On the contrary, one study reported that the similar success rates between patients with VLPP below 60 cmH2O and with VLPP above 60 cmH2O; success rates were 74.2% and 67.2%, respectively [9]. Another study compared 61 women with MUCP less than 20 cmH2O and 204 women with MUCP above 20 cmH2O and the cure rates between two groups were 77% and 86%, respectively, with no statistical differences [10].
In our study, the cure rates were 76.7% in ISD group and 75.3% in non ISD group after minimum three year follow-up, and there was no significant difference. These cure results were similar to success rates of previous studies and suggest that TVT is an effective treatment even in women with ISD after long term follow up with other studies [9,10].
There is few data on factors influencing the outcome after mid urethral sling in ISD patients, including urodynamic findings. Paick et al. [2] analyzed 61 ISD women and reported that urge symptoms and low MUCP were independent factors for treatment failure.
Low MUCP as a prognostic factor was reported by other study [11] and Liapis et al. [3] reported low success rate in women with 'fixed' urethra. These results mean that adequate cooptation or mobility of the urethra is important for a successful outcome of the procedure.
Our results showed that the only VLPP was the significantly different between the subgroups of ISD patients. The mechanism of this result is probably that the lower VLPP means the more damaged components of the continence mechanism such as the external sphincter, levator musculature, pubourethral ligaments, urethropelvic ligaments, and urethra elasticity.
The major limitations of the study include the relatively small number of patients and the lack of objective outcome measures. Also, there was a possibility of selection bias during follow-up. Although low VLPP was only significant factor with TVT procedure failure in ISD patients, larger number of patients is needed to justify this results.
Despite of our limitations, our study has strong point in terms of long follow-up duration and identification of another prognostic factor of TVT in ISD patients.
Our findings suggested that ISD women can have successful long-term surgical outcomes after TVT procedures. However, clinicians should consider the possibility of TVT procedure failure in ISD women who have extremely low VLPP.
Notes
No potential conflict of interest relevant to this article was reported.