INTRODUCTION
Lower urinary tract symptoms (LUTS) represent a common condition associated with diminished quality of life, and more than half of men and women experience some kind of LUTS in their lifetime. In general, the typical symptoms of overactive bladder (OAB) and urinary incontinence (UI) are storage symptoms, and OAB and UI are considered to be more prevalent in women than in men. However, women also experience voiding symptoms such as a weak urinary stream, intermittency, and terminal dribbling [
1,
2]. Therefore, women complaining of voiding symptoms can be diagnosed with female voiding dysfunction (FVD), such as bladder outlet obstruction (BOO) and detrusor underactivity [
3,
4]. Moreover, previous studies have reported that some women experience both storage and voiding symptoms at the same time. Irwin et al. [
1] reported that 8% of women showed both storage and voiding symptoms. Other researchers also showed that 14.5% of women experienced storage and voiding symptoms and, interestingly, women with voiding symptoms were likely to experience storage and postmicturition symptoms. The reason why women present with complex symptoms such as storage and voiding LUTS is that various conditions such as OAB, UI, and FVD often coexist and symptoms of OAB can exist secondary to BOO [
5]. Thus, there is a need for research on FVD associated with BOO in women with storage symptoms.
Clinically, some women with storage LUTS also have BOO; therefore, OAB treatment fails in these women. According to a study where urodynamic studies (UDS) were performed in women with refractory OAB, BOO was observed in 27% of women and detrusor overactivity (DO) was observed in 38.7%. BOO was associated with the severity of frequent micturition, nocturia, and a weak urinary stream. Multivariate analysis showed that the severity of frequent micturition was a predictor of BOO [
6]. These findings indicate that not all women complaining of symptoms of OAB are real OAB patients and that storage symptoms such as frequency and nocturia can be common LUTS in women with BOO. As a result, women with BOO can be misdiagnosed with OAB, and it is necessary to perform UDS to identify BOO in women.
For women with OAB, UDS is not recommended when considering behavioral and medical treatment [
7]. However, a longitudinal prospective follow-up study by Verghese et al. [
8] reported improved therapeutic outcomes in women with OAB symptoms or urgency-predominant mixed UI after they received urodynamic-based treatment. Women with urgency-predominant mixed UI showed better outcomes than women with OAB symptoms and DO. These results demonstrated that UDS-based treatment decisions help to reduce symptoms and that UDS plays an important role in women with complex symptoms.
There are few studies about the urodynamic characteristics of female BOO patients who are initially diagnosed with OAB based on their symptoms; therefore, we analyzed urodynamic parameters in women with functional BOO and investigated differences compared with women with OAB and with stress urinary incontinence (SUI).
MATERIALS AND METHODS
This retrospective study (from January 2015 to December 2017) included 108 women (over 20 years old and without any underlying conditions that would influence LUTS) with storage LUTS and functional BOO diagnosed by UDS. All women were initially diagnosed with OAB; however, OAB treatment failed. Therefore, they received UDS for a functional evaluation. Seventy-eight women with SUI included in this study were diagnosed by a clinical history, physical examination, and UDS. Thirty-four women with OAB who underwent UDS were included. The diagnostic criteria of female BOO were as follows: maximum flow rate (Qmax) < 15 mL/s, combined with detrusor pressure at Qmax (PdetQmax) > 20 cm H
2O in a pressure-flow study. The exclusion criteria were as follows: neurological deficiency; anatomical cause of obstruction; previous pelvic, spinal, or anti-incontinence surgery; intake of drugs affecting voiding; urinary tract infection; and systemic disease (diabetes, hypothyroidism). All patients underwent assessments, including a detailed urogynecological history, a physical examination, urinalysis, urine culture, and multichannel UDS unless the patient responded to anticholinergic treatment. The urodynamic study included uroflowmetry, postvoid residual volume (PVR) determination, a cystometrogram, and a pressure-flow study. The urodynamic techniques and measurements, terms, and diagnostic criteria conformed to the recommendations of the International Continence Society [
9].
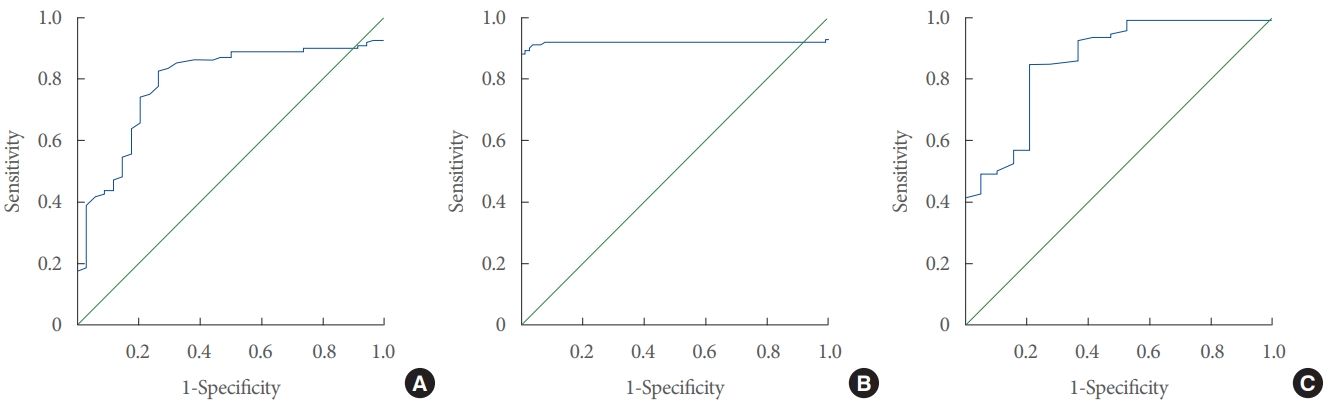
Statistical analyses were performed using IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA). Analysis of variance was used to determine if significant differences were present among women with OAB, BOO, and SUI, and the Tukey test was used to determine which groups had significant differences from each other. Additionally, receiver operating characteristic (ROC) analysis was conducted to analyze the parameters that we measured as diagnostic tools. A 5% level of significance was used for all statistical tests.
DISCUSSION
In this study, women with OAB symptoms and FBOO who were diagnosed by UDS showed a low Qmax, a lower voiding volume, and a higher PVR than women with SUI or women with OAB. Women with storage symptoms and FBOO showed typical urodynamic findings of BOO, such as an increased PdetQmax and MUCP. The lower MCC and DO observed in women with FBOO were secondary changes in bladder function induced by BOO. Therefore, these findings induce storage symptoms. Interestingly, 17.6% of women with FBOO experienced IC/BPS at the same time. Women with FBOO exhibited a higher MUCP than women with FBOO and IC/BPS. In addition, DO was only noted in women with FBOO only. However, women with both FBOO and IC/BPS had a lower MCC than women with FBOO. However, the PdetQmax exhibited low predictive value for differentiating women with both IC/BPS and FBOO from women with FBOO only. Based on these results, for the first time, we suggest MUCP as a potential biomarker for establishing the underlying cause in women who do not respond to symptom-based treatment.
The prevalence of BOO in women has been reported from 2.7% to 23% and is caused by pelvic organ prolapse, urethral stricture, anti-incontinence surgery, FBOO, and dysfunctional voiding [
10-
14]. Studies on female BOO are not sufficient compared with studies on men with BOO associated with benign prostatic hyperplasia. However, some studies have investigated the diagnosis and treatment of female BOO. Choi et al. [
14] found that 12.8% of women who visited urologic clinics due to LUTS were diagnosed with female BOO. Their most common LUTS was incomplete bladder emptying, and the second most common symptom was frequency. Moreover, most women with BOO showed both storage and voiding symptoms rather than complaining of isolated voiding or storage symptoms [
10,
11]. Similar to these results, the total International Prostate Symptoms Score, the voiding subscore, and the storage subscore were not significantly different between women with BOO and OAB [
15]. Symptoms of OAB are sometimes not reliable for diagnosis in women with LUTS [
16-
18]. Therefore, a detailed evaluation of LUTS and UDS is important to avoid overlooking BOO in women who report OAB symptoms.
Compared with those of OAB and SUI patients, the characteristic findings of UDS in women with FBOO in the present study were a lower MCC, a lower DO, and a higher MUCP. The lower MCC and DO observed in women with FBOO are factors that induce OAB symptoms. Several studies have demonstrated that a decreased MCC contributes to inducing storage symptoms. FitzGerald et al. [
19] and Sekido et al. [
20] observed that frequency and UI were associated with a lower MCC in women with OAB. In addition, Cho et al. [
14] found a lower MCC in women with BOO, similar to the results of the present study. Although few studies have investigated DO in women with BOO, 2 previous studies showed that DO was observed in 12.6% and 49.9% of women with BOO, respectively [
6,
16]. In the present study, DO was noted in 35.2% of women with FBOO. DO is associated with urgency and urge UI as well as symptom severity [
6,
15]. Therefore, women with DO induced by BOO are likely to experience OAB symptoms. In general, the diagnostic role of MUCP is considered low, and no studies have assessed the value of MUCP for predicting female BOO. We noted that MUCP in women with SUI (30.2±7.3 cm H
2O) was similar to that in previous reports by Weber (women with SUI: 39.4±24 cm H
2O) [
21]. Moreover, MUCP in women with FBOO was significantly higher than that in women with OAB and SUI; therefore, MUCP might have diagnostic value. Although PdetQmax has diagnostic value for discriminating BOO in women, some patients cannot complete the pressure-flow study due to emotional distress. Thus, MUCP may help to diagnose BOO in women who cannot urinate during a pressure-flow study [
22].
Interestingly, 19% of women with FBOO had IC/BPS, and this is the first report of IC/BPS found in women with FBOO. In contrast, some investigators have analyzed the urodynamic characteristics of women with BOO and IC/BPS. Cameron and Gajewski [
23] observed that 48.1% of women with IC/BPS had BOO according to a pressure-flow study, and others reported that 60.1% of women with IC/BPS showed symptoms of bladder outlet dysfunction, such as dysfunctional voiding, poor relaxation of the external urethral sphincter, and bladder neck dysfunction, according to a video urodynamic study [
24]. In addition, their IC/BPS patients with BOO showed a lower bladder capacity, a smaller voided volume, a larger PVR, a higher PdetQmax, and a lower Qmax than IC/BPS women without BOO. Similar to these previous findings, women with FBOO and IC/BPS in the current study showed a lower voided volume and bladder capacity than women with FBOO only. However, a lower MUCP was observed in women with FBOO and IC/BPS than in women with FBOO only. Moreover, the Qmax and PdetQmax were not significantly different. From these results, we infer that the decreased bladder capacity in women with FBOO and IC/BPS was associated with pain in comparison with women with FBOO only. The lower MUCP in the women with FBOO and IC/BPS might have also been influenced by IC/BPS. There have not been enough studies defining the underlying mechanism of the coexistence of BOO and IC/BPS; however, some researchers have proposed possible hypotheses such as pelvic floor hypertonicity. Pelvic floor spasms and impairments in pelvic muscle relaxation have been observed in both BOO and IC/BPS [
25,
26].
Women with FBOO had significantly different MUCP values from those in women with OAB and SUI. Moreover, a significant difference in MUCP was noted between women with FBOO only and women with FBOO and IC/BPS. Therefore, MUCP might be a potential biomarker for FBOO in women with OAB symptoms. From these results, we suggest a cutoff value of MUCP for the prediction of FBOO. In OAB women, an MUCP ≥ 87 cm H2O might be a predictor of FBOO, and in women with SUI, an MUCP ≥36 cm H2O might be a predictor of FBOO. Since PdetQmax had poor predictive value for the differentiation of women with FBOO and IC/BPS from women with FBOO without IC/BPS, an MUCP ≥92 cm H2O might be a predictor for FBOO in women with FBOO and IC/BPS. Although we found a possible role for MUCP as a prediction tool, there are limitations to the general application of our suggested cutoff value of MUCP because the current definition of FBOO is diverse among clinicians. However, MUCP could help to identify FBOO in women with complex LUTS.
In conclusion, women with storage symptoms and FBOO showed different urodynamic findings compared with women with OAB and women with SUI. Moreover, some women simultaneously had FBOO and IC/BPS. Therefore, special interest in patients who complain of LUTS is necessary because LUTS is associated with various underlying conditions, and UDS should be performed in patients in whom OAB medication fails. For the first time, we reported that MUCP could have predictive value for identifying FBOO in women with complex LUTS.