Overview of the Epidemiology of Lower Urinary Tract Dysfunction in South Korea
Article information
Abstract
This review assessed the epidemiology of voiding dysfunctions in South Korea. Comprehensive understanding of this epidemiology is crucial because the senior population and the social burden are increasing because of voiding dysfunctions is growing. We searched the medical records using several terms related to voiding dysfunction: benign prostatic hyperplasia, urinary incontinence, lower urinary tract symptoms, overactive bladder, and nocturia. We then estimated the prevalence of voiding dysfunctions in South Korea; our data were comparable with those from other countries, with slight differences. The ranges of incidences varied widely between studies, mostly because investigators defined disorders differently. Voiding dysfunction greatly affects healthcare costs and individual quality of life; therefore, more proper and valuable epidemiologic data are needed. In addition, efforts to unify the definitions of various voiding dysfunctions and progress in investigational methodologies using multimedia are warranted.
INTRODUCTION
Voiding dysfunction is highly prevalent among older people. For instance, urinary incontinence (UI) affects about one third of healthy elderly people, and up to 90% of nursing home patients [1]. The proportion of the elderly population is increasing worldwide; it is currently around 10%, and is expected to reach 20% within 40 years [2].
Accordingly, the prevalence of conditions such as metabolic syndrome and obesity are increasing annually, and these are key risk factors for voiding dysfunction. Moreover, voiding dysfunction influences patient quality of life, and can contribute to serious morbidities, such as falls and bone fractures [3]. Therefore, the various dysfunctions in urination confer a huge socioeconomic burden.
The average age of the South Korean population is increasing more rapidly than that in other countries: the proportion of elderly people rose from 3.8% in 1980 to 9.5% in 2006 [4]. Consequently, South Korean society is becoming more concerned over voiding problems after middle age. For this reason, it is essential that investigators conduct epidemiologic studies into the prevalence of voiding dysfunctions in South Korea. In this review, we aimed to clarify the prevalence and clinical features of voiding dysfunctions among both men and women.
Several extensive epidemiologic studies have been performed in Western countries since the 1990s; however, in South Korea, epidemiologic studies have only been conducted since the start of the 21st century.
To advance epidemiologic research, we have proposed a number of possible study methodologies for experimental epidemiologic studies. Longitudinal designs confer greater statistical power than cross-sectional designs, because longitudinal research uses serial data that reveal substantial realistic prevalences, as well as the potential causes of the disease. On the other hand, longitudinal studies take longer and are more expensive. For this reason, more epidemiologic studies involve a cross-sectional design.
To ensure significant epidemiologic data, investigators must select a proper target population and adopt proper survey methods; questionnaires should be adjusted to the target population.
Early epidemiologic studies into voiding dysfunction were mainly performed by postal survey; this method has been commonly used since the 1960s. This approach involves lower costs and higher efficiency, and it has fewer effects on the patients’ mood; therefore, the postal survey served as a strong epidemiologic method. More recently, communication devices and multimedia technology have allowed telephone interviews and internet surveys to emerge as practical epidemiologic tools. Telephone interviews can provide a cross section of almost the entire population, and they are cost- and time-effective. Furthermore, the results of telephone interviews are less influenced by the interviewer than are those of personal interviews [5].
Nonetheless, this method is limited, because, in the past, few people in South Korea had telephones. With the increased distribution of telephones, this method has become more popular. From a methodological point of view, the telephone interview can be affected by social desirability bias, which can arise in cases of delicate personal questions, especially in the field of urology. Furthermore, some people feel their privacy is violated by random-dialing surveys; therefore, the nonresponse rate increases [6].
After high-level communication and multimedia technology were developed, the internet survey was introduced to gather data. However, such an approach confers a coverage problem, because most people are still not capable of accessing surveys via the internet or electrical devices [7]. For this reason, the internet survey must be developed further if it is to become the ideal survey design. In addition, internet surveys require comprehensive programming, which is not true of face-to-face interviews.
Therefore, the face-to-face interview is still frequently used in epidemiologic studies, even though more money, time, and manpower are required. The major advantage of the personal interview is that the researcher can explain the intent and exact meaning of questions; this guarantees higher response quality.
It is true that every survey method has its own advantages and handicaps, and sometimes various survey methods are used concurrently. Nonetheless, large-scale epidemiologic data are most frequently obtained by telephone interview or internet survey.
Voiding dysfunction is mostly caused by benign prostatic hyperplasia (BPH) in men. Furthermore, in both sexes, UI, lower urinary tract symptoms (LUTS), overactive bladder (OAB), and nocturia are highly prevalent, distressing conditions. Herein, we have provided an overview of the epidemiologic studies into the above voiding dysfunctions in South Korea. We tried to focus on nearly all significant studies in the country. All of the surveys included in this review were conducted after profound consideration of the various aspects. Furthermore, we have reviewed in detail each specific survey method, as well as the methods for obtaining detailed clinical details of voiding dysfunction. Finally, we considered the practical limitations of the survey selection processes, which are influenced by special factors.
BENIGN PROSTATIC HYPERPLASIA IN SOUTH KOREAN MEN
BPH is the most prevalent urologic condition in older men. Its various voiding-related symptoms, enhanced by obstruction of the bladder outlet, include nocturia, tenesmus, urgency, and hesitancy; these symptoms reduce the quality of life in affected men. The prevalence of BPH increases with age, and it affects 40% to 70% of men aged between 60 and 70 years [8,9].
BPH is diagnosed pathologically in approximately 40% of autopsies of men in their 50s, and in 70% of autopsies of men in their 60s. However, traditionally, BPH has been identified clinically on the basis of symptoms. Hence, in this review, we have used based based definitions of BPH as a voiding dysfunction.
To investigate the real prevalence of BPH, we must clarify the diagnostic criteria. In this regard, the demarcation of what constitutes clinical BPH is somewhat controversial; to date, clinicians have come to no consensus regarding the definition of BPH. In addition, different characteristics of the target population, as well as the methods used to collect information, can influence the results. This diversity in the definition of BPH influences the ability of investigators to analyze and compare results across studies.
Table 1 lists the BPH-focused epidemiologic studies we included. The first study into BPH prevalence in the inland area of Chungcheongbuk-do was performed in 1999, and 27.7% of 764 men were found to be affected [10]. In this study, BPH was defined when the prostate volume (PV), measured by transrectal sonography, was ≥20 mL, and when the maximal flow rate (Qmax) was ≤10 mL/sec.
In another study, BPH was defined when the International Prostate Symptom Score (IPSS) was ≥8, when the PV (measured by finger) was ≥30 mL, and when Qmax was ≤15 mL/sec. The rate of moderate-to-severe IPSS was 49.5% (213 in 431 men). But by the definitions in this study, BPH prevalence were 4.3% of men in their 50s, 13.2% of men in their 60s, and 16.3% of men in their 70s or older (overall, 11.1% of men aged over 50 years). The population-adjusted prevalence of BPH in South Korean men aged 50 and over was 8.7% [11].
Another community-based study defined BPH in cases of an IPSS ≥8 points and a Qmax ≤10 mL/sec; the study found that the incidence of BPH was 25.5%. On the basis of IPSS, 36.3%, 49.7%, and 14.0% of the men were mildly (1–7), moderately (8–19), and severely (20–35) symptomatic, respectively [12].
In 2009, Park et al. [13] found that the prevalence of BPH, defined in cases of an IPSS >7 and a PV >30 mL, was 40%. This study was based on the Korean Longitudinal Study on Health and Aging, a population-based, prospective study involving a randomly sampled population of 301 men aged >65 years living in Seongnam, South Korea.
In the latest study, which involved 779 men who lived in Yangpyeong County and participated in a prostate examination campaign, BPH was defined when IPSS was ≥8 points and PV was ≥25 mL. Such a definition is consistent with the standards of the Korean Urological Association. The prevalence of BPH was found to be 20.0% [14].
The wide range of BPH prevalence in previous studies — from 11% to 40%—is mainly due to methodological differences between studies, such as differences in selection of the target population. Furthermore, the proportion of the population who are elderly is higher in some districts than in others. The diagnostic descriptions of BPH are also diverse.
The prevalence of clinical BPH in South Korea is similar to that in Western and other Eastern countries. Specifically, the BPH prevalence in Scotland was estimated as 25.3% in 705 men [9]. A cross-sectional study involving 8,466 Iranian men (>40 years old) conducted by 74 personal interviewers identified a prevalence of 23.8% when BPH was defined as an IPSS >7, a Qmax of <15 mL/sec, and a PV >30 mL [15].
Asians mostly show similar or worse symptom scores than Caucasians. Asian data were collected from China, South Korea, Singapore, Pakistan, the Philippines, India, Thailand, and Taiwan. The prevalences of an IPSS ≥8 points were 18%, 29%, 40%, and 56% among men in their 40s, 50s, 60s, and 70s or older, respectively. These rates are higher than those reported for the United States (12% 17%, 23%, and 29%, respectively) [16]. This may be due to differences in the cellular composition of prostatic tissue between Asians and Caucasian-Americans. Some studies have reported that Asians have more portions that are glandular and less muscle and connective tissue, as well as a transition zone that occupies a higher volume ratio within the prostate. However, studies use various combinations of parameters to define BPH, including symptom score, PV, and urodynamic parameters. Therefore, it remains difficult to determine the exact in prevalence, and to make further progress in the survey method.
URINARY INCONTINENCE IN SOUTH KOREA
Even though UI is not life threatening, it is a severe health problem and causes psychological distress, hygiene problems, and social impairment in affected patients and their families [17]. According to the International Continence Society definition, any involuntary leakage of urine constitutes UI [18].
In general, many women regard UI as a natural consequence of childbirth and aging. Even though UI can be managed in various ways by clinicians, many women tend to manage their UI personally. In addition, due to shame, many people conceal their problem rather than ask for medical help. So then, the reported prevalence of UI varies widely due to cultural discrepancies [19]. The incidence of UI increases with aging, and with the rapid growth of the aged population, UI is gradually becoming an enormous social burden in South Korea.
Table 2 shows the studies into UI prevalence. The earliest prevalence data for UI in South Korea were reported in 2004; the study comprised an internet survey involving 3,372 respondents, and the prevalence of UI in women was 21% [20]. An additional large telephone survey reported that the overall prevalence of UI was 40.8% among 1,301 women. With regard to UI type, 22.9% of cases were stress-type, 3.1% were urgetype, and 14.9% were mixed [21].
In 2008, the Korean National Survey on Urinary Incontinence yielded nationwide representative data; in this survey, 13,345 households were interviewed. The prevalence of UI was 24.4%, and stress UI was the most prevalent type [22]. A further population-based cross-sectional telephone survey of South Koreans included 888 men and 1,112 women. The overall prevalence of UI was 2.9% in men and 28.4% in women. The most predominant types were other (1.3%) in men and stress (20.7%) in women. Stress UI affected 0.9% of men and mixed-type UI affected 4.1% of women [23].
Data from 9,873 women participants in the Korea National Health and Nutrition Examination Survey were reported in 2014. This study reported that the overall prevalence of UI among women was 7.9%. By age, the prevalences were 10.1% and 10.3% in women over 40 and 60 years of age, respectively. The reported prevalences were 0.8%, 4.6%, 9.3%, 10.8%, 10.9%, and 9.7% among women in their 20s, 30s, 40s, 50s, 60s, and 70s or older, respectively [24].
The ‘2008 Actual Living Conditions of the Elderly and Welfare Need Survey’ obtained data by personal interview; this survey attempted to provide longitudinal population information using a cluster sampling method. These data were reported in 2015. Of the 8,961 women studied, 6.5% had self-reported UI and 2.3% had been medically diagnosed with UI [25].
The most recent population-based, cross-sectional study randomly sampled 500 Korean women who reside in the Seoul, Incheon, and Gyeonggi-do areas. The survey comprised a computer-aided telephone interview, and used 16 questions to collect data; the questions sought information on demographic characteristics, information sources, disease insights, and general health-seeking behavior. Among the responders, 23.8% of women experienced UI [26].
Current reviews of UI show that the worldwide incidences vary from 25% to 45% [27,28]. Western data report a prevalence range of 3.9% to 24.4% in women [29], while Asian data have shown variable results: 53.7% of Japanese women aged over 40 years, and 27.7% of Taiwanese women aged 65 years or older [30].
Korean data on UI have also varied widely; however, the prevalence is comparable with that of worldwide data, irrespective of region or race. Because Korea is a conservative country, and Koreans are relatively passive in coping with UI problems, UI may be more common among South Korean women than is reported. Therefore, assessment of the real UI prevalence is the first step to creating public awareness and increasing public knowledge regarding this problem. In this way, we may be able to improve control of this disorder.
OVERACTIVE BLADDER IN KOREA
OAB is a broad terminology that refers to a complex of symptoms such as urinary urgency, urge incontinence with nocturia, and frequent urination. Investigation into the prevalence of OAB is still in its infancy, because the definitive characters of OAB are obscure in that there is no clear metabolic or histologic explanation for the symptoms [31]. Nonetheless, OAB is a common voiding dysfunction, especially among older people. In addition to causing physical problems, OAB may have a negative effect on the person’s emotions and quality of life; furthermore, the disorder may eventually place a severe financial burden on society—not only in medical terms, but also through loss of productivity.
The reported incidence of OAB has varied significantly among epidemiologic studies, because the diagnostic criteria with regard to each individual urological symptom are different. In South Korea, epidemiologic studies into OAB that had consistent diagnostic criteria began relatively recently, as did studies into the impact of the condition on the individual and society.
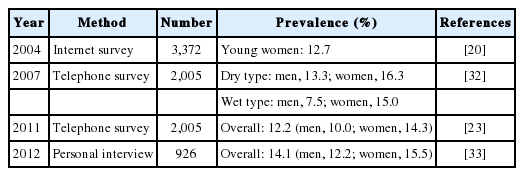
We summarized the South Korean studies into OAB in Table 3. In 2004, 3,757 participants completed a questionnaire via an internet survey. Among the 3,372 women who responded, 429 suffered from OAB (12.7%) [20]. In another study, nationwide community samples were obtained from South Koreans aged 40 to 89 years. Through a telephone survey that used allocation sampling, Choo et al. [32] reported that the prevalence rates in men and women were 13.3% and 16.3% for dry-type OAB, and 7.5% and 15.0% for wet-type OAB, respectively.
In 2011, Lee et al. [23] performed a population-based survey using the International Continence Society (ICS) definition of OAB. The study was cross-sectional in design and used a telephone survey method to gather data from 2,005 persons. They found that 12.2% of individuals had OAB, with similar rates among men (10.0%) and women (14.3%).
In a regional study in Guri City and Yangpyeong County, Gyeonggi-do, the general OAB prevalence was 14.1% (12.2% in men and 15.5% of women). The survey involved face-to-face interview of 926 residents, and defined OAB when the urgency score was >2 points and the OAB Symptom Score was >3 points [33].
In general, South Korean prevalence data range from 10% to 16%, with a higher rate in women than in men. This is similar to the prevalence found in Western countries; furthermore, the prevalence of OAB in South Korea increases with age, just as in Western countries. For instance, in a survey involving 5,204 Americans, the prevalence of OAB was 16.0% in men and 16.9% in women [34]. Data from six European countries revealed that the overall prevalence of OAB among 16,776 people was 16.6% [35]. Referring again to Asia, the prevalence among 4,570 Japanese respondents was 12.4%, and it was 20.9% among 1,247 Taiwanese women [36,37].
OAB patients are known to have a lower quality of life; however, investigators require a deeper insight into the condition’s harmful influence in the community, especially in South Korea. Proper epidemiologic data will be a valuable resource for educating the South Korean population about OAB—a term unfamiliar to the public at the current time.
LOWER URINARY TRACT SYMPTOMS IN SOUTH KOREA
According to the 2002 ICS definition, the term “LUTS” encompasses various types of storage, voiding, and postmicturition symptoms [31]. Similar to other voiding dysfunctions, LUTS are a common condition, and their prevalence has positive correlations with age [38,39]. One problem with LUTS prevalence studies is that the condition is difficult to define, and most studies use criteria that overlap with those of BPH, UI, or OAB. Until recently, only a few studies had used the 2002 ICS definitions of LUTS. Moreover, there are considerable discrepancies between different epidemiologic studies into LUTS.
When investigation into LUTS prevalence began, one innovative study involving South Korean men was performed in Yeoncheon County. This community-based epidemiologic study assessed the severity of urinary symptoms in 514 men over 50 years of age. The overall incidence was 23.2%: 17.7% in those aged 50–59 years, 23.3% in those aged 60–69 years, and 35.3% in those aged over 70 years [40].
In 2001, Cho et al. [41] defined LUTS using the IPSS. A total of 1,356 men between 40 and 79 years old living in the Seoul area were selected using stepwise random sampling and surveyed with a questionnaire that included questions about IPSS. About 16% had moderate-to-severe LUTS, defined as an IPSS >7. The prevalence of moderate-to-severe LUTS increased significantly with age, 10%, 16%, 29%, and 45% in the age groups 40–49, 50–59, 60–69, and 70–79 years, respectively.
One population-based telephone survey involving 2,000 individuals reported that the overall frequency of LUTS was 61.4% (53.7% in men, 68.9% of women). Storage LUTS affected 44.6% of men and 64.4% of women, voiding LUTS affected 28.5% of men and 25.9% of women, and postmicturition LUTS affected 15.9% of men and 13.9% of women. Storage LUTS are therefore more common than voiding and postmicturition LUTS [23].
Kim et al. [42] surveyed a random sample of men older than 40 years. All respondents were asked to report the presence of LUTS in a questionnaire. Responses from 1,842 men were investigated, and the overall prevalence of LUTS was 83.4%. Storage LUTS (70.1%) were more common than voiding (60.4%) or postmicturition LUTS (38.3%).
As can be seen in the above summary, the reported prevalences of LUTS vary widely, from 16% to 83%. Nonetheless, the South Korean prevalence data regarding LUTS are comparable to those in reports from across the world. Furthermore, even the wide-ranging data corroborate the results from previous reports. One study in Europe found that the prevalences of LUTS were 16.2%–25.1% in men and 12.6%–23.7% in women [43]. Another Western population-based study reported a 64.3% incidence among 19,165 individuals [29]. Asian prevalence data regarding LUTS are also diverse, ranging from 14% to 59%. Moderate-to-severe LUTS were reported by 36% of men aged 50–59 years, 50% of men aged 60–69 years, and 60% of men aged 70–79 years [44].
However, there have been fewer epidemiologic studies into LUTS in Asian countries than in Western countries, and prevalence data focus mainly on men rather than on the general population; there are few data regarding the prevalence in women. As shown in Table 4, the prevalence varies widely between studies worldwide, mainly because investigators still have no clear definition of LUTS. The condition is complex, and this is a severe obstacle to researchers who wish to obtain the true epidemiology of LUTS in South Korea.
NOCTURIA IN SOUTH KOREA
Nocturia is the one of the leading causes of distress among voiding dysfunctions. Nocturia is defined by the ICS as the “complaint that the individual has to wake at least once at night to void” [31]. Getting up at night to void urine increases the risk of individual physical or mental injuries in elderly people. Nocturia reduces the quality of life and is associated with sleep fragmentation, reductions in productivity, reduced general health, and falls or fractures [45].
The diagnostic criteria for nocturia are still controversial. Most urologists consider a single episode to be nocturia, but many epidemiologic studies have defined nocturia as more than two episodes of voiding per night [46,47].
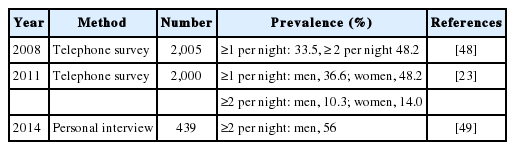
Only a few studies into nocturia have been conducted in South Korea (Table 5). In 2008, Choo et al. [48] conducted a clinically validated, computer-assisted telephone survey. Among the 2,005 respondents (1,005 women and 1,000 men), 33.5% complained of once-per-night voiding, and 48.2% stated that they had to void twice or more per night. Interestingly, even though the prevalence of nocturia was high, the negative influence on everyday life was reported to be minimal.
In 2000, data were published involving 2,000 participants (888 men and 1,112 women). According to this cross-sectional telephone survey, the prevalences of nocturia ( ≥2 voids per night) were 36.6% in men and 48.2% of women [23].
In 2012, Lee et al. [49] investigated the prevalence of nocturia (≥2 voids per night) using a face-to-face interview method. The prevalence was 56.0% in this community-based study involving 439 elderly South Korean men in a single city (Seongnam).
It is true that not all patients suffer from nocturia, and the degree of impact is influenced by the severity of the condition. To understand the exact epidemiologic nature of nocturia in South Korea, it will be useful to examine to what degree cultural background has an effect on the psychological impact of nocturia [50,51].
The prevalence of nocturia in South Koreans appears to be higher than that in other communities. The prevalences of nocturia (≥2 voids per night) among Japanese community-dwelling adults were 28.1% in men and 27.1% in women [52]. A multistage, cluster sampling study with a personal interview-type design was used to obtain data from 15,988 people in the United States. The study indicated that 33.1% of men and 32.6% of women experience ≥1 voids per night, and that 15.5% of men and 20.9% of women experience ≥2 voids per night [53]. In The Netherlands, a telephone survey involving 4,721 people was conducted. The prevalences of nocturia ( ≥2 voids per night) were 9% in men and 16% in women [54]. Data collected from 1,247 women and 1,221 men in Austria showed that 37.2% of men and 43.1% of women experienced ≥1 voids per night, and that 7.5% of men and 8.1% of women experienced ≥2 voids per night [55].
These lower prevalences in other populations may have been affected by the population distributions studied, as well as by the definition of nocturia used. Nonetheless, the probable causes of the high prevalence of nocturia among South Koreans remain to be clarified.
DISCUSSION
Epidemiologic surveys are essential for understanding the potential causes and characteristics of related medical disorders. In addition, they are the necessary first steps in evaluating psychosocial impacts of a disorder.
In general, most of the estimated prevalences of voiding dysfunctions in South Korea were similar to those in other countries; they varied widely, primarily due to different definitions of the respective disorder. In addition to the lack of solid definitions of voiding dysfunctions, inconsistencies in integrated questionnaires and variances among target populations render population-based surveys difficult to compare.
Most investigations were based on self-reported symptoms, so recall bias and person-to-person social bias may have been present, especially in personal interviews. Nonresponse bias could also be a problem in that nonresponders to a survey may have been significantly different from responders in terms of the respective symptoms.
Population-based surveys are carried out because diagnosis by strict medical assessment is not practical in such large-scale prevalence studies. Nonetheless, researchers need to develop other ways to obtain more proper, valuable epidemiologic data.
We think that investigators should focus on unifying all of these disease entities and definitions. More efficient investigational processes and methodologies are also warranted.
From a methodological point of view, 14 of the studies (58.3%) included in the present report, involved personal interview data. Despite considering the advantages of the personal interview, the ratio is relatively still high. However, the bashful and conservative nature of Koreans may prevent investigating the epidemiology of voiding dysfunction in simpler, less time-consuming ways. As a result, only eight telephone surveys and two internet surveys were available. Relatedly, the random digital dialing in telephone surveys is often perceived as violating personal privacy; for this reason, telephone surveys will not be easy to conduct in the future.
Due to the noteworthy progress in multimedia technology in South Korea, epidemiologic studies using the internet and other applications are a promising method. Using web services, respondents can reply to the survey anywhere and at any time. An internet survey can gather enormous amounts of data from large groups within a relatively short time. Furthermore, videos or pictures can be used easily, at reasonable cost, and with less social desirability bias than the other study methods. Mobile communication techniques may improve methothologic efficiency in various social and natural science fields, as well as in medicine. For example, bladder diary apps may exclude the disadvantages of pen-and-paper diaries in clinical application [56]. Currently, the apps available vary in quality, but there is room for medical associations to collaborate with developers in this area.
Even though some of the public are not familiar with surveys by internet or electrical devices, much progress will be made in epidemiologic studies due to technology, especially with regard to methodology [7].
This review constituted a nationwide representative summary of studies on the prevalence of voiding dysfunctions in South Korea. We hoped to contribute to the understanding of voiding dysfunctions by providing the epidemiologic characteristics of each condition. However, much work remains to be done in this field, because few surveys had a longitudinal design, and more investigations are needed that consider the whole range of age, sex, and location in the South Korean population.
CONCLUSION
Given the influence of voiding dysfunction on quality of life, as well as the socioeconomic burden of the condition, more studies on the optimal approaches to epidemiologic study will be needed in the future. These should include technical improvements in methodologies.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.