The Current State of Artificial Intelligence Application in Urology
Article information
Abstract
Artificial intelligence (AI) is being used in many areas of healthcare, including disease diagnosis and personalized treatment and rehabilitation management. Medical AI research and development has primarily focused on diagnosis, prediction, treatment, and management as an aid to patient care. AI is being utilized primarily in the areas of personal healthcare and diagnostic imaging. In the field of urology, significant investments are being made in the development of urination monitoring systems in the field of personal healthcare and ureteral stricture and urinary stone diagnosis solutions in the field of diagnostic imaging. In addition, AI technology is also being applied in the field of neurogenic bladder to develop risk monitoring systems based on video and audio data. This paper examines the application of AI to urological diseases and discusses the current trends and future prospects of AI research.
INTRODUCTION
Artificial intelligence (AI) is being utilized across the healthcare system in all areas, including the development of medical robots, diagnosing and treating diseases, and more. The rapid adoption of healthcare AI is expected to improve the quality of healthcare facilities and services in the near future, extending the lives of patients and improving their quality of life. The rise of AI is one of the biggest technological advancements in history, and from smartphones to surgical robots, AI has changed society in monumental ways. As AI technology continues to advance, its application in healthcare will only expand. AI in medicine can be divided into 2 types: virtual and real. Virtual AI includes information science and systems-based learning, such as managing symptoms to make treatment decisions based on deep learning. Physical AI includes robotics and nanotechnology to improve drug delivery. Both areas of AI can contribute to dramatic improvements in patient care. These new tools and capabilities will have a much-needed impact, especially in urology.
In the era of the Fourth Industrial Revolution, harnessing the exponential growth of data is increasingly recognized as a matter of industrial competitiveness. Most industries are struggling to process the flood of information and data more efficiently and productively, and successfully meeting this challenge is seen as a matter of business survival. As a result, AI is growing in importance as a way to easily analyze vast amounts of information [1]. As the focus of AI shifts from simply utilizing data to generating new information and knowledge and developing and evaluating services, its application in the healthcare industry is also expanding. Many organizations and countries are investing heavily in healthcare AI because the adoption of AI technology in healthcare can have far-reaching effects on society.
The application of AI will be useful in many areas of urology, including benign urological conditions and cancer, especially in analyzing large amounts of data for diagnosis and prognosis. Machine learning (ML) is a branch of AI that integrates statistics and algorithms to find relationships in data. These tools can be applied to clinical data to create powerful risk models and redefine the classification of diseases. As medicine evolves into the “big data” era, with increasing amounts of complex medical data, ML can be a powerful resource for exploring, explaining, and applying information. The application of AI in various medical fields is beginning to take off, and urology is no exception, with AI research actively pursued across the entire cycle of analysis, diagnosis, treatment, and management of urological conditions. Most of these studies are conducted as an adjunct to patient care and treatment, with model research being a key technology.
In this paper, we will introduce cases in the field of urology where these AI technologies have been applied. We believe that this will increase the possibility of applying AI in each field and give a vision of the future application of AI to urological diseases.
AI TRENDS FOR URINARY DISEASES
Medical AI research and development is primarily focused on diagnosis, prediction, treatment, and management as an aid to patient care. AI is primarily being utilized in personal healthcare and diagnostic imaging. In the field of urology, a lot of investment is being made in the development of urination monitoring systems for personal healthcare and diagnostic imaging solutions for ureteral strictures and urinary stones. There are also cases of AI technology being applied to neurogenic bladders. In this paper, we will cover some examples in each of these fields and discuss the prospects for AI applications.
AI Applications in Urologic Disease Diagnosis
AI research is being conducted on various urological diseases, including prostatic hyperplasia, ureteral stricture, urinary stones [2-10], and urinary tract infections. AI is mainly used as an aid for clinicians to diagnose diseases, and it is essential to verify the effectiveness of applying AI technology through many clinical trials. As a result, we were able to identify fields and technologies with high applicability in the medical field, and in this paper, we introduced some of the major cases by technology field.
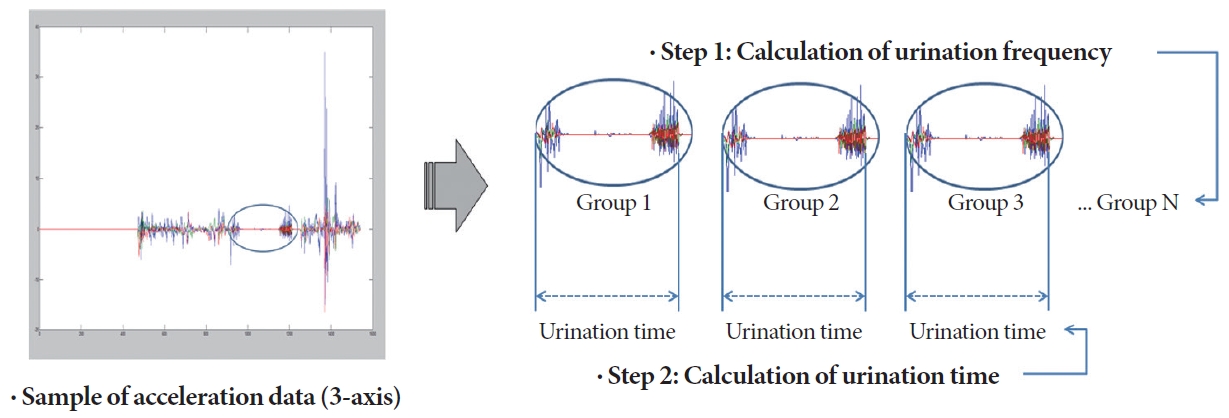
First, researchers at Gachon University Gil Hospital developed an assistive technology that can help diagnose urinary diseases by analyzing urination posture, or movement signals, collected through gyro and accelerometer sensors [11]. First, the research team developed a urination diary app that supports the automatic creation of urination diaries for patients with urinary diseases. The urination of male users was categorized into 3 periods: before, during, and after urination, so that the frequency, duration, and volume of the user’s urination could be automatically analyzed through learning and recognition. The technical basis of the app is AI learning and urination behavior recognition, and various ML and deep learning techniques were used for this purpose. Figs. 1 and 2 show the research process and concepts.
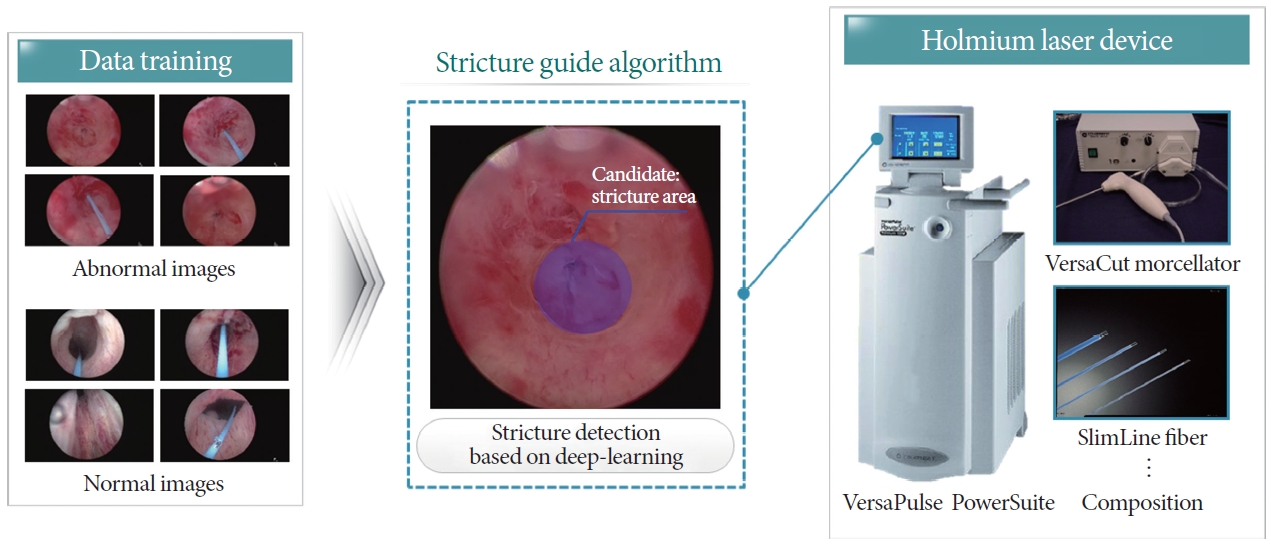
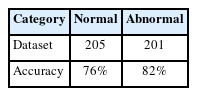
Researchers at Sejong Chungnam National University Hospital are working on a technology that utilizes image data from microendoscopy, computed tomography (CT), etc. to assist in the diagnosis of conditions such as ureteral stricture and urinary stones [12]. Research on diagnostic aid for ureteral strictures is important because it is often difficult to identify the area of stricture during surgery, making it difficult to remove the stricture. For decision support, AI technology is used to automatically recognize the area of stricture in ureteral images obtained through microendoscopy to assist clinicians during surgery. The AI technology used utilizes deep learning techniques such as ResNet-50 to provide recognition information in real time [13-17]. Fig. 3 shows a concept map of this study. In addition, since accurate diagnosis is paramount for the surgery and treatment of urolithiasis, research is also underway to support the diagnosis of urolithiasis by utilizing abdominal CT and Carm imaging data. To support the diagnosis of urinary stones, research is underway on a technology that automatically diagnoses urinary stones and evaluates their condition based on image data [12]. For this purpose, research is being conducted to explore the optimal technology method in terms of image processing (Watershed), machine learning (support vector machine), and deep learning (ResNet-50, Fast-RCNN [18]). Fig. 4 shows a concept map of this research.

Concept map of research on an algorithm for urolithiasis recognition. CT, computed tomography; IRB, Institutional Review Board; AI, artificial intelligence; CNN, convolutional neural network; RNN, recurrent neural network; LSTM, long short-term memory; IoU, intersection over union.
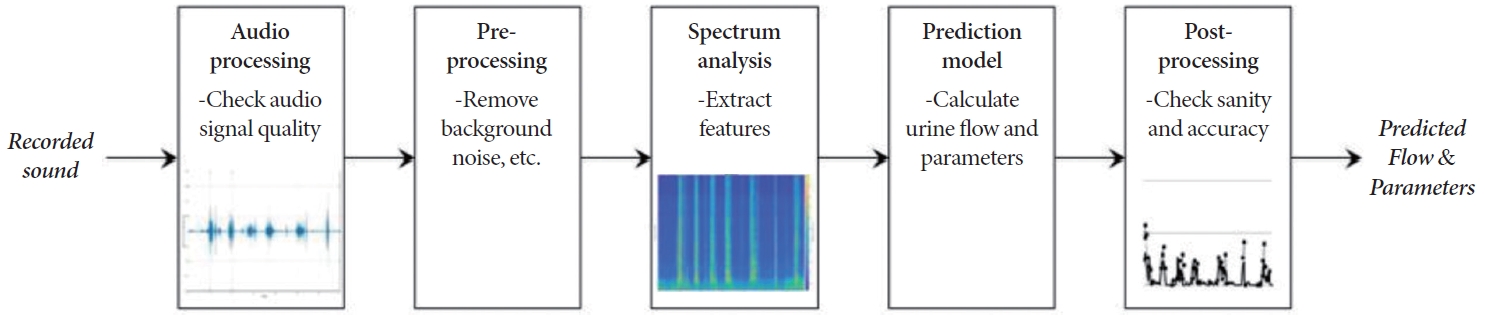
In addition, researchers at Seoul National University Bundang Hospital developed a mobile urethral flow measurement technology through acoustic signal analysis. In 2017 and 2018, they conducted an internal performance evaluation of the urinary flow measurement technology through clinical trials to confirm its validity software (SW) with this technology is an acoustic analysis-based urinary flow measurement software, which was registered as a class 2 medical device with the U.S. Food and Drug Administration (FDA) in 2020. The technology measures urination patterns based on acoustic analysis and AI, enabling noninvasive testing with a smartphone. Based on the sound produced when urine hits water, it automatically records urination volume, peak flow rate, urination time, etc. and displays the data in a data graph and stores the measurement data in a dashboard. AI technologies such as linear/nonlinear regression analysis, classification analysis, and deep learning have been applied here. Fig. 5 shows the workflow of this device.
AI Applications for Neurogenic Bladder
Neurogenic bladder refers to overactive bladder, a condition in which patients diagnosed with abnormalities in bladder storage function by dynamic testing, such as stroke patients, develop bladder overactivity due to nerve damage. Existing studies [19, 20] have reported that stroke affects the symptoms or disease presentation of neurogenic bladder. There are several of these patterns, among which the pattern of facial paralysis is easy to identify. The asymmetry criterion of the face is mainly important, and precise detection of it is essential to prevent stroke. In this study, we analyze the early symptoms of stroke through ML-based recognition [21] of facial images collected by detecting facial paresis symptoms in stroke patients.
In addition to providing various light sources, they also provide various image format conversion technologies required for diagnosis. In addition, as it targets the elderly, it is possible to install AI analysis software that can accurately diagnose the early stages of stroke so that it can be utilized in daily life. The experimental test environment proposed in this paper is as follows: a software that analyzes images obtained from face and arm motion videos and displays suspected stroke images based on AI learning (object). Among the analyzed results, it supports the function of detecting and capturing objects in the acquired face and arm motion images, which can be used as reference indicators for stroke diagnosis. Among the video frames, still cuts are taken by selecting frontal shots, facial landmarks, eyebrows and eyes, corners of the mouth, and lip frames. During the experiment, one of the precursor symptoms of stroke patients is that the face is not symmetrical from side to side due to paralysis on one side of the face. In order to use these features to distinguish patients from normal people in the input image, we need to extract features from 2 groups of face databases to learn the difference. We need to detect the angle and tilt to calculate the distance between feature points in the face region and compare the left and right differences to calculate the degree of asymmetry. Since existing databases have different sizes and tilts of face regions, we need to go through a preprocessing process to normalize the size and angle of the detected faces. Then, to obtain the rotation angle, we store the left effect values of the left and right end landmarks as the rotation angle. We store an affine transformation matrix to align the image using this rotation angle. After applying the angle to extract landmarks from the rotated image, calculate the distance values to find features for left-right symmetry analysis. To extract the calculated distance values into meaningful data, we divide and compare the left and right distances and store the larger value, and also extract calculated values such as slope, angle, and ratio of eyebrows and lips. The extracted data is then normalized, labeled, and trained with a convolutional neural network (CNN) model.
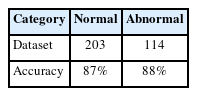
They found that the training accuracy averaged 86% and the validation accuracy averaged 83%, and the accuracy of the control and patient groups was also close to 80%. We recorded the accuracy and loss as a function of the number of epochs, and found overall similar performance on the training data. The results are shown below (Tables 1, 2). Specifically, the classification accuracy of the patient data was 88% and the control data was 87%, which can be seen in the following tables (Tables 3, 4). In the end, we found that using AI to diagnose stroke quickly and accurately had an indirect, if not a direct, positive effect on the neurogenic bladder.
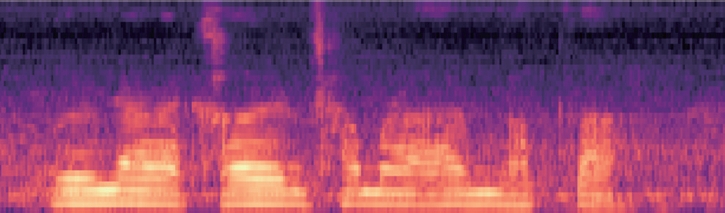
This is the second study [22] of neurogenic bladder, and it is a case of judgment based on speech data rather than images. In the case of speech, this includes inaccurate pronunciation or unnatural intonation, and accurately detecting these patterns is crucial for stroke prevention. In this research case, we propose a platform that can precisely analyze the speech of stroke patients with neurogenic bladder and detect them in advance to prevent the disease. Digital therapy in the field of neurogenic bladderrelated stroke management is a type of software therapy that changes a patient’s behavior or lifestyle through a series of digital stimuli such as images and sounds, and collects and analyzes data accordingly. Currently, the application of digital therapies is gradually expanding to fields related to behavior and habit change, such as mental illness and chronic diseases. Digital therapies can serve as a complement to conventional medications in conditions that require ongoing management. The SW proposed in this study can provide scientific monitoring feedback to users or surrounding nursing personnel by iteratively learning and analyzing the utterance data of stroke patients and expressing continuous feedback and interest. The SW in this study is an AI SW that acquires specific sentence speech data of stroke clinical patients and analyzes it to warn of early stages of neurogenic bladder-related stroke. It extracts feature values by analyzing the input speech and converts them into stroke indexes and stores them. The stored stroke index is classified into learned stroke indicators and finally displays whether a stroke has occurred. The input speech is processed for feature analysis with the mel-frequency cepstral coefficient (MFCC) algorithm, and a CNN learning algorithm is used to extract the speech disorder index and derive classification values by index. The MFCC algorithm is used to extract feature data from speech to learn the differences between patients and normal people.
Fig. 6 shows the main feature spectrum of the MFCC algorithm, which is the result of the feature vectorization process based on the input voice data, and finally, through voice stroke symptom detection, risk factors can be identified in advance and notification services can be provided, and the user’s results can be stored in the DB and used for retraining.
Fig. 7 shows the data processing flow chart for performance evaluation. It tested the analytical model by processing 30 abnormal data and 30 normal data in real time. The results showed high test accuracy of 98.7% for normal data and 99.6% for abnormal data. Table 5 shows the final test results.
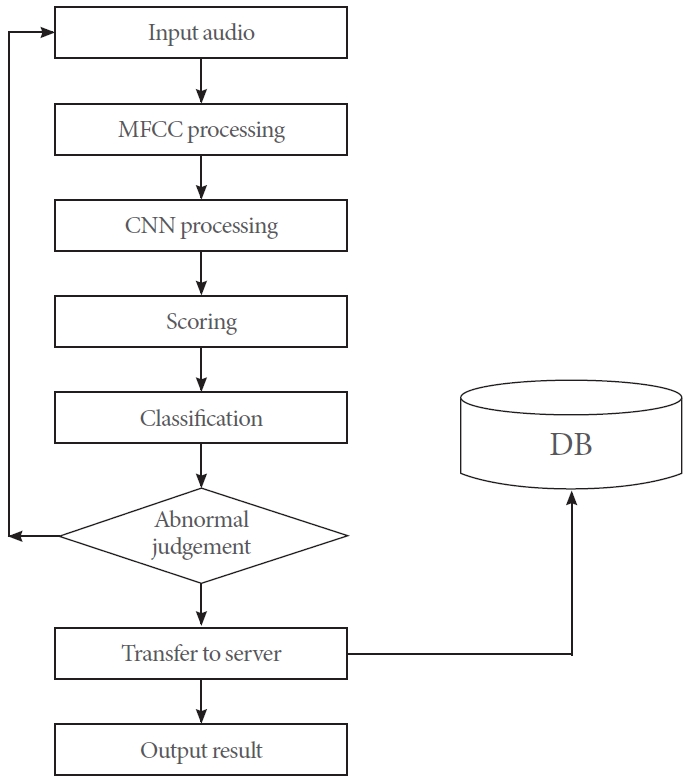
The data processing flow chart for performance evaluation. MFCC, mel-frequency cepstral coefficient; CNN, convolutional neural network; DB, database.
CONCLUSION
In this paper, we presented examples of applications of AI technology to urinary system diseases, and discussed current trends and future directions. To do so, we reviewed domestic and foreign cases and studies on personal healthcare services and disease diagnosis assistance. First, studies that focused on disease diagnosis and analysis assistance mainly focused on recognizing specific diseases, such as ureteral strictures and urinary stones. Based on image analysis of strictures and stones, this research aims to determine the presence or absence of disease and perform morphological analysis, such as assessing the location of problematic areas, to help clinicians make a final diagnosis and support surgery. In addition, research on the application of AI to the field of neurogenic bladder disease has also been conducted. These have mainly been monitoring systems that seek to identify conditions based on video and audio data, and proactively alert patients to risks.
These AI applications were mainly focused on signal analysis and image analysis for various purposes such as disease prediction, management, diagnosis, and analysis. The level of AI technology used was mostly high, and various advanced AI technologies are being researched based on representative analysis techniques such as recurrent neural networks for signal analysis and CNNs for image analysis.
In addition, there are many challenges to be solved, such as effectiveness verification and medical device certification, in order for various AI-based disease support services to be properly applied in the medical field. There are procedural requirements beyond the R&D level, such as commercialization through institutional investment, effectiveness verification through clinical verification, and medical device certification by the U.S. FDA and the Korean Ministry of Food and Drug Safety. In other words, for successful commercialization and practical use, costs other than those spent on R&D must be considered. It seems that we have already passed the stage of verifying the applicability of AI to urological diseases in the field. In the future, more R&D support from various organizations is needed to ensure that AI technology is properly applied at home and in the medical field.
Notes
Grant/Fund Support
This study was conducted with the support of the government (The pan-ministerial medical device project group) in 2023 (Korea Medical Device Development Fund, No. RS-2020-KD000188, Development of intelligent complex biological information-based monitoring device for the management of neurological diseases and mental health for the elderly).
Research Ethics
This research was approved by the Institutional Review Board of Gachon University Gil Medical Center (approval number: GAIRB2021-483).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION STATEMENT
· Conceptualization: ESK
· Data curation: SJE
· Formal analysis: ESK
· Funding acquisition: ESK
· Methodology: SJE
· Project administration: ESK
· Visualization: SHY
· Writing - original draft: ESK
· Writing - review & editing: SHY