Diagnostic Tool for Assessing Overactive Bladder Symptoms: Could the International Prostate Symptom Storage Subscore Replace the Overactive Bladder Symptom Score?
Article information
Abstract
Purpose
The goal of this study was to compare the International Prostate Symptom Storage Subscore (IPSS-s) and the overactive bladder symptom score (OABSS) as tools for assessing the symptoms of overactive bladder (OAB).
Methods
A cross-sectional study was conducted of a sample of 1,341 patients aged 50 years and older with lower urinary tract complaints who had undergone a medical examination at one of several centers. For each patient, we reviewed the International Prostate Symptom Score and the OABSS. The patients were divided into 2 groups according to their IPSS-s result (group 1, score ≥6; group 2, score<6) and into another 2 groups according to their OABSS diagnosis (group 3, OAB patients; group 4, non-OAB patients). We determined whether the OABSS varied to a statistically significant extent between groups 1 and 2. Furthermore, we evaluated the correlation of IPSS-s severity with the OABSS results in group 3, and the OAB diagnosis rate was compared between groups 1 and 2.
Results
In groups 1 and 2, the OABSS results were not found to vary to a statistically significant extent (P=0.326). In group 3, no significant correlation was found between IPSS-s severity and the OABSS results (P=0.385). In the prevalence analysis, no statistically significant difference was found among the groups, and the receiver operating characteristic curve showed an area under the curve of 0.474.
Conclusions
The results of this cross-sectional analysis suggest that the IPSS-s and the OABSS are not significantly correlated. Although both scores are used to measure OAB symptoms, the simultaneous use of IPSS-s and OABSS is not warranted.
INTRODUCTION
Overactive bladder (OAB) is defined as urinary urgency, with or without urge incontinence and usually with frequency and nocturia, in the absence of an infection or other obvious pathologic conditions [1]. Since OAB is defined by subjective rather than objective symptoms, the patient’s perspective is important in managing this disease.
For this reason, several diagnostic tools evaluating patient-reported outcomes are available. The overactive bladder symptom score (OABSS) is based on a validated self-assessment questionnaire consisting of 4 questions assessing OAB symptoms. Patients respond to each question about their bladder symptoms during the previous week. The OABSS provides an overall composite score, as well as individual scores [2].
However, the International Prostate Symptom Score (IPSS) is the most commonly used assessment tool for men with lower urinary tract symptoms (LUTS) [3,4]. The IPSS consists of a total of 7 questions on voiding symptoms (incomplete emptying, intermittency, weak stream, and straining to void) and storage symptoms (frequency, urgency, and nocturia).
Generally, many clinicians employ the IPSS to assess patients complaining of LUTS. Moreover, when the chief complaint is urgency or urge incontinence, clinicians tend to investigate OAB using the International Prostate Symptom Storage Subscore (IPSS-s) [5]. However, the relationship of the OABSS to the IPSS has not been sufficiently evaluated. It is not unusual for the IPSS-s alone to be used for assessing OAB. In the present study, we compared the IPSS-s and the OABSS as tools for assessing OAB.
MATERIALS AND METHODS
Patient Sample and Data Collection
A cross-sectional retrospective study was conducted, with a total sample of 1,341 patients. We enrolled patients older than 50 who voluntarily underwent a free medical checkup at the Health Promotion Center in Seoul from 2012 to 2014. The following inclusion criteria were used: patient age older than 50 years, good overall mental and physical health, and LUTS complaints. We reviewed the IPSS and OABSS results for each patient. The patients were divided into 2 groups according to their IPSS-s result (group 1, score ≥6; group 2, score <6) and into another 2 groups according to their OAB diagnosis (group 3, OAB patients; group 4, non-OAB patients) based on the OABSS criteria [6].
Assessment Tools
International Prostate Symptom Score
The IPSS was adapted from the American Urological Association symptom index and quality of life questionnaire and has emerged as the standard tool for the evaluation of symptoms of benign prostatic hyperplasia (BPH) [3]. The symptom index consists of 7 questions on incomplete emptying, urinary frequency, intermittency, urgency, weak urinary stream, hesitancy, and nocturia. In this tool, a total score of 0–35 is calculated by summing the scores of 0–5 for the 7 questions. The quality of life index is scored on a scale of 0–6, according to the patient’s symptoms.
Overactive Bladder Symptom Score
The OABSS is based on a symptom assessment questionnaire designed to quantify OAB symptoms as a single score, and contains questions about the following 4 symptoms of OAB: daytime frequency, nighttime frequency, urgency, and urge incontinence. In this tool, the patients are asked to rate their symptom severity on a Likert scale with the maximum (worst) scores of 2, 3, 5, and 5. The total score ranges from 0 to 15, and a more severe OAB is indicated by a higher score. The scoring system is designed to place more weight on urgency and urgency incontinence than on frequency. The questionnaire has been shown to satisfy psychometric criteria for reliability [2].
Statistical Analysis
Continuous variables were expressed as the mean±standard deviation, median (interquartile range), or as the number (percentage) of cases. Categorical variables were reported as the number and percentage. The Student t-test and Spearman correlation coefficient were used for the statistical comparisons of categorical and continuous variables, respectively. The chi-square test was used to investigate the prevalence of various conditions between groups. Furthermore, receiver operating characteristic (ROC) curves were used to assess the ability of the IPSS-s to predict OAB diagnoses according to the OABSS diagnostic criteria. All analyses were performed with IBM SPSS Statistics ver. 20.0 (IBM Co., Armonk, NY, USA). P-values <0.05 were considered to indicate statistical significance.
RESULTS
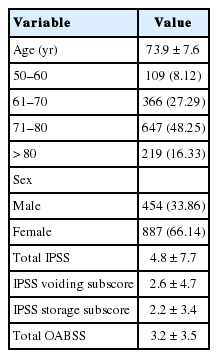
The patients’ mean age was 73.9±7.6 years, and their age distribution is presented in Table 1. The mean total IPSS, IPSS-voiding subscore, IPSS-s, and OABSS results were 4.8±7.7, 2.6±4.7, 2.2±3.4, and 3.2±3.5, respectively.
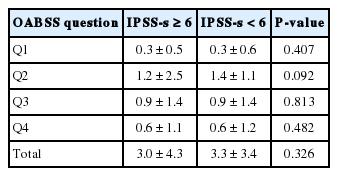
The results of the comparison of OABSS results between groups 1 and 2 (defined according to their IPSS-s results) are shown in Table 2 (Student t-test). None of the 4 questions of the OABSS questionnaire showed a significant result; similarly, the total OABSS did not significantly differ between these 2 groups (P=0.326). Additionally, we compared urgency symptom scores with the total OABSS, and likewise found no statistical significance (P=0.616).
Furthermore, the correlation of the IPSS-s severity with OABSS results was investigated in groups 3 and 4 (defined on the basis of OAB diagnoses). All correlation coefficients were negative or not statistically significant (total OABSS; P=0.385, r=−0.048) (Table 3).
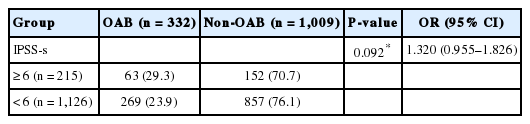
We evaluated the OAB diagnosis rate in patients grouped according to their IPSS-s results (score ≥6 vs. score <6) using the chi-square test, and found no statistically significant difference (P=0.092; odds ratio, 1.320; 95% confidence interval, 0.955–1.826) (Table 4). Moreover, a ROC curve was constructed to assess the ability of the IPSS-s to predict the diagnosis of OAB according to the OABSS diagnostic criteria. The area under the curve was 0.474 (P=0.160) (Fig. 1).
DISCUSSION
This analysis compared the OABSS and the IPSS-s in order to determine whether the IPSS-s can be used as a replacement tool for the OABSS. We found no significant correlation between the IPSS-s and the OABSS, which means that the simultaneous use of the 2 tools should be avoided.
The assessment of LUTS is indispensable for an accurate diagnosis, the proper choice of treatment, and evaluating the efficacy of treatment of lower urinary tract disorders. For patients complaining of LUTS, the IPSS questionnaire has often been used as a symptom assessment tool [7-9]. Many urologists use the IPSS in daily practice in investigations of LUTS in both female and male patients [10-13].
However, although an IPSS-s result of ≥6 is somewhat meaningful, whether it can be used for assessing OAB is still controversial. This may be because the IPSS was originally designed for the assessment of BPH symptoms [3]. Some studies have argued that the IPSS-s can be used for evaluating storage LUTS; however, scant evidence supports the use of the IPSS-s for assessing OAB [5].
In our study, the patients were divided into 2 groups according to a high or low storage subscore. No significant correlations were found between each question of the OABSS questionnaire and the IPSS-s, or for the total OABSS. The above results may indicate that even a high IPSS-s may not be useful for diagnosing OAB.
Furthermore, we evaluated the correlation between IPSS-S severity and the OABSS, and likewise found no statistically significant results. As discussed above, the composition of the questionnaire is slightly different in these 2 diagnostic tools. Frequency, nocturia, and urgency are common items in both questionnaires, but urge incontinence is only included in the OABSS questionnaire.
Considering the small differences in the questionnaire composition, it was unexpected that the 2 diagnostic tools were not found to be correlated. The OABSS places more weight on the scores for urgency and urgency incontinence (maximum score, 5) than on micturition frequency (maximum score, 2 or 3). For OAB patients, the most bothersome symptom is urgency or perhaps urge incontinence (when the latter symptom is present) [14,15]. These considerations may explain the discrepancy between these diagnostic tools.
The OABSS was developed and validated in order to collectively express OAB symptoms as a single score [16]. Since OAB is a collection of symptoms, evaluating all the symptoms, rather than a single or a limited number of symptoms, may be expected to show better performance in the assessment of symptoms and their changes. Therefore, the reason for sometimes using the IPSS-s instead of the OABSS may be that OAB symptoms have usually been quantified by counting episodes of micturition, urgency, and nocturia. However, the diagnosis rate of OAB was not significantly higher in the group with a high storage subscore than in the group with a low storage subscore. Moreover, we found the IPSS-s to be an insufficient indicator in diagnosing OAB due to its relatively low area under the curve (0.474) in the ROC analysis.
This study has some limitations. First, this was a cross-sectional investigation of a Korean population with clinical diagnoses involving a relatively small number of patients. Therefore, our results may not be generalizable to other populations. Second, the current study may have been affected by selection bias. Prospective studies with a larger number of patients are warranted to confirm the present results, which suggest that the IPSS-s cannot replace the OABSS as an assessment tool for OAB, and that the indiscriminate use of both questionnaires should be avoided.
Notes
Research Ethics
This study was conducted in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments, and the appropriate ethical review boards approved this retrospective study (AS13030).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.