Effects of Acute Sacral Neuromodulation at Different Pulse Widths on Bladder Overactivity in Pigs
Article information
Abstract
Purpose
Sacral nerve stimulation has been used to treat overactive bladder. This study evaluated the effects of stimulation using different pulse widths on the inhibition of bladder overactivity by sacral nerve stimulation (SNM) in pigs.
Methods
Implant-driven stimulators were used to stimulate the S3 spinal nerve in 7 pigs. Cystometry was performed by infusing normal saline (NS) or acetic acid (AA). SNM at pulse widths of 64 μsec to 624 μsec was conducted at the intensity threshold at which observable perianal and/or tail movement was induced. Multiple cystometrograms were performed to determine the effects of different pulse widths on the micturition reflex.
Results
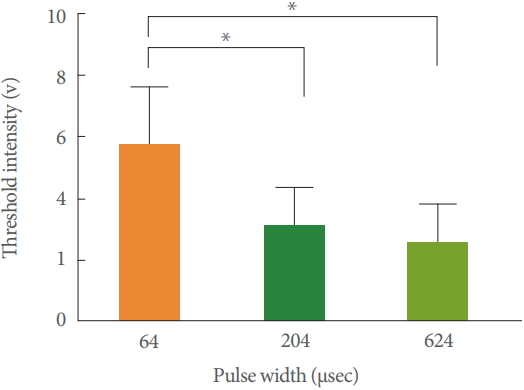
AA-induced bladder overactivity reduced the bladder capacity to 46.9%±7.1% of the NS control level (P<0.05). During AA infusion, SNM at 64 μsec, 204 μsec, and 624 μsec increased the bladder capacity to 126.1%±6.9%, 129.5%±7.3%, and 140.1%±7.6% of the AA control level (P<0.05). No significant differences were found among the results obtained using pulse widths of 64 μsec, 204 μsec, and 624 μsec (P>0.05). The actual intensity threshold varied from 0.7 to 8 V. The mean intensity threshold (T visual) for pulse widths of 64 μs, 204 μs, and 624 μs were 5.64±0.76 V, 3.11±0.48 V, and 2.52±0.49 V. T visual for pulse widths of 64 μsec was larger than the other two T visual for pulse widths of 204 μsec and 624 μsec (P<0.05). No significant differences were found among the T visual for pulse widths of 204 μsec and 624 μsec (P>0.05).
Conclusions
This study indicated that different pulse widths could play a role in inhibiting bladder overactivity. It is not yet certain which pulse widths increased bladder capacity compared with AA levels, to minimize energy consumption and maintain patient comfort during stimulation, 204 μsec may be an appropriate pulse width for SNM.
• HIGHLIGHTS
- Different pulse widths may play a role in inhibiting bladder overactivity.
- It is not yet certain which pulse widths are best, more pulse widths, especially of 64 μsec to 300 μsec, need to be investigated in the future.
- To minimize energy consumption and maintain patient comfort during stimulation, 204 μsec may be an appropriate pulse width for SNM.
INTRODUCTION
Overactive bladder (OAB) is a syndrome of the urinary tract symptoms of urgency, with or without urinary urge incontinence, usually with frequency and nocturia, in the absence of infections or other local pathological factors [1]. Lower urinary tract dysfunction affects millions of people worldwide and severely impacts quality of life [2]. Many patients do not respond to medications such as anticholinergic drugs owing to lack of adherence, efficacy, or tolerability or side effects [3]. Sacral nerve stimulation (SNM) offers a safe and minimally invasive method to treat voiding dysfunction, especially in patients with conditions refractory to conventional therapies [2]. Potential for response to SNM therapy can be tested by implanting a permanent tined quadripolar lead at the sacral foramen during an outpatient surgical procedure, testing the lead for 2 weeks as an outpatient, and then evaluating response. If symptoms improve by at least 50%, an implantable pulse generator can be placed during a second surgical procedure [4]. A potential reason for unsatisfied clinical effects of sacral nerve stimulation could include the use of stimulation parameters were inappropriate. An assessment of the stimulation parameters should be performed to achieve better clinical outcomes [5].
The stimulation parameters include stimulation intensities, frequencies, pulse width and so on. Many studies have proved that the optimal intensity and frequency of electrical stimulation [6-9].
Pulse width, one of the parameters of the stimulation field, has not been as well screened [10]. Currently, pulse widths are typically adjusted at 180 to 240 μsec (e.g., 210 μsec, Medtronic InterStim VR Therapy, Implant Manual) for human SNM [10]. Some experts believe that there is little potential for achieving significant motor nerve fiber recruitment selectivity by varying the stimulus pulse width over the clinically useful range of 50 μsec to 500 μsec when surface stimulation is used [11]. Some experts believe that shorter pulse widths will provide more efficient therapy delivery and increased longevity of the stimulator [10]. Identification of the optimal stimulation pulse width is important in clinical neuromodulation.
The goals of this study were to determine whether bladder inhibition or excitation could be induced by SNM using different stimulation pulse widths and to find the optimal pulse widths which would achieve better clinical effect. We investigated the effects of acute SNM delivered using an implant-driven stimulator (SacralStim, General Stim, Inc., Hangzhou, China) on the micturition reflex in pigs.
MATERIALS AND METHODS
Animals
Seven adult Guizhou miniature pigs (3 males, 4 females) were used for this study. The animals were 21 to 27 months old (mean±standard deviation [SD], 23.1±1.95 months) and weighed 60 to 75 kg (mean±SD, 68.1±4.7 kg) at the time of implant.
Device Introduction
The stimulation parameters (SacralStim) are 0 to10 V, a frequency rate of 5 to 110 Hz, and a pulse width of 30 to 630 μsec. These parameters can be adjusted using the remote control. When we test it in studies, we find that the shortest and longest pulses were 64 μsec and 624 μsec, respectively, due to machine limitations. Thus, we chose 64 μsec, 204 μsec, and 624 μsec to identify the appropriate pulse width for SNM.
Surgical Implantation
We preanesthetized pigs by an intramuscular injection of ketamine hydrochloride (10 mg/kg) and the pigs were maintained with isoflurane (2%–5% in oxygen) by tracheal cannula connected to an anesthesia machine (Matrx VMR; Midmark, Dayton, OH, USA). We used the electro-cardiscope monitor (Cardell 9500; Midmark) to monitor the heart rate and blood oxygen level. In a prone position, the surgical field was aseptically prepared. We made a 7- to 8-cm incision from the middle of both posterior superior iliac spines to the tail. Based on our experience, only the S3 foramen of pigs can be penetrated by the localizing needle. The stimulating electrodes (Model ISL-280620 SacralStim) with 6 contact points were passed into each needle introducer. The introducers were removed and the electrodes were sutured (Fig. 1). We confirmed the successful placement by the perianal and/or tail motor responses when energizing the stimulating electrode with an external stimulator by gradually increasing the voltage. Then, an extension cable (Model EL-1006 SacralStim) was tunneled in the upper buttock and connected to the stimulator (Model IS-10A SacralStim). All incisions were closed with sutures. Although the pigs were implanted bilaterally (for another study), only the left sides of stimulation were used in this study.
Cystometry and SNM testing
Acute experiments were conducted at least 1 day after implantation. We preanesthetized the pigs with an intramuscular injection of ketamine hydrochloride (10 mg/kg). Anesthesia was induced with intravenous α-chloralose (62.5 mg/kg) and maintained with intravenous α-chloralose (50 mg/kg/hr) after 1 hour. We used the electro-cardiscope monitor (Cardell 9500; Midmark) to monitor the heart rate and blood oxygen level throughout the experiment. Fluid was administered via the ear vein.
We exposed the urethra via the inferior margin of the pubis and introduced an 8F three-lumen catheter (Cook Company, Spencer, IN, USA) into the bladder through the urethra. The catheter was then secured by a ligature around the urethra. One lumen of the catheter was connected to a pump and used to infuse the bladder with normal saline (NS) or acetic acid (AA) at a rate of 30 mL/min. one lumen used to measure the bladder pressure was connected to a pressure transducer (Andromeda Urodynamic System, Taufkirchen/Potzham, Germany). The last lumen used to measure the urethral pressure was closed (Fig. 2). Methods, definitions, and units conformed to the International Continence Society standards [12]. Stimulation was performed after completing the preparation work.
Stimulation Protocol
Before stimulation, impedance was measured to check device integrity. A fixed frequency (14 Hz) was delivered to the sacral nerve. The intensity threshold for inducing perianal and/or tail movement was determined by gradually increasing the stimulation intensity. Bladder capacity was used for testing the inhibitory effect of the stimulator. The bladder was drained before each experiment. After the appearance of the first sharp, largeamplitude bladder contraction, bladder infusion with NS or AA was stopped, and this infusion volume was defined as the bladder capacity.
After emptying the bladder, we first performed 2 or 3 cystometrograms (CMGs) with NS without stimulation to obtain the control bladder capacity. Then, after emptying the bladder, 2.5% AA was infused into the bladder to irritate and induce bladder overactivity for 3 to 5 CMGs. After the bladder capacity stabilized, SNM (64 to 624 μsec pulse width) was applied during sequential CMGs. The actual intensity threshold varied among pigs. Response thresholds were obtained from visual detected threshold (T visual). The bladder was emptied after each CMG, and a 5-minute rest period was given between successive CMGs to allow the distended bladder to recover.
Statistical Analysis
IBM SPSS Statistics ver. 19.0 (IBM Co., Armonk, NY, USA) was used for the statistical analysis. The significance level was set at P<0.05. Repeated measurements of the same animal under the same CMG conditions were averaged. All summary data were expressed as mean±standard error. Statistical significance was determined by paired t-test or one-way analysis of variance (ANOVA) followed by a least significant difference test. The paired t-test was performed between the NS and AA groups to compare the repeated CMG recordings. The bladder capacities of the AA group were normalized to the measurement of the first control and CMG during NS instillation. The bladder capacities of the SNM groups (64 μsec, 204 μsec, 624 μsec) were normalized to the CMG of AA. One-way ANOVA was performed for different CMG conditions (AA, 64 μsec, 204 μsec, 624 μsec) and T visuals with different pulse widths.
RESULTS
Inhibitory Effects of Different Pulse Widths SNM on Bladder Overactivity Induced by AA Irritation
Table 1 and Fig. 3 summarize the bladder capacity of the NS, AA infusion, SNM at 64 μsec, 204 μsec, and 624 μsec conditions in 7 pigs. We successfully created a model of OAB in pigs for AA induced overactivity and reduced BC compared with the NS control levels. Different pulse widths (64 μsec, 204 μsec, and 624 μsec) increased the bladder capacity compared with the AA control level. Due to the large variability of bladder capacity for pigs, we compared with the percentage of their own bladder capacity.

The bladder capacity of the normal saline, acetic acid infusion, SNM at 64 μsec, 204 μsec, and 624 μsec conditions in 7 pigs

Summarized the bladder capacity of the normal saline, acetic acid infusion, sacral nerve stimulation at 64 µsec, 204 µsec, and 624 µsec conditions in 7 pigs. NS, normal saline; AA, acetic acid.
Irritation of the bladder with 2.5% AA induced bladder overactivity and significantly reduced the bladder capacity to 46.9%±7.1% of the NS control level (427.2±126.0 mL) (P<0.05) (Figs. 4, 6). During AA infusion, SNM at 64 μsec, 204 μsec, and 624 μsec all significantly increased the capacity to126.1%±6.9%, 129.5%±7.3%, and 140.1%±7.6% of the AA control level (P<0.05) (Figs 5, 6). No significant differences were found among the results obtained using pulse widths of 64 μsec, 204 μsec, or 624 μsec (P>0.05) (Fig. 5).
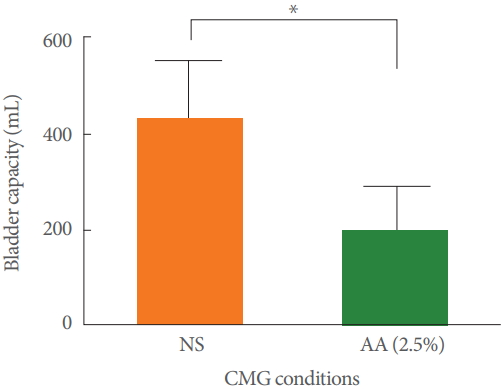
Summarized capacity results of acetic acid irritation. Irritation of the bladder with 2.5% acetic acid significantly reduced bladder capacity compared with the normal saline control level (*P<0.05). NS, normal saline; AA, acetic acid; CMG, cystometrogram. *Statistically significant difference.
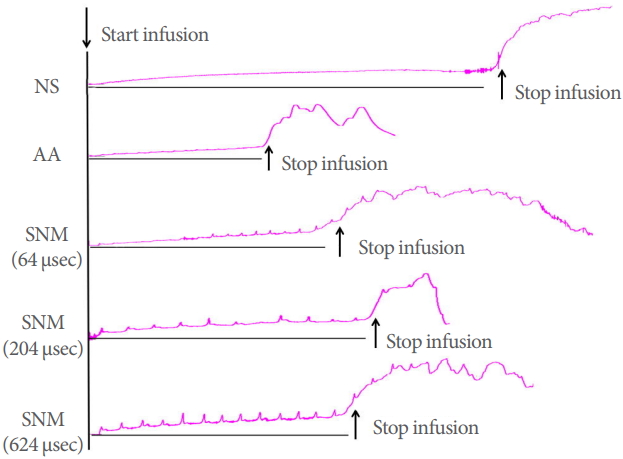
Sacral nerve stimulation was given over a range of pulse widths to suppress bladder overactivity induced by intravesical infusion of 2.5% acetic acid. The black bars under the pressure trace indicate the stimulation duration. The short arrows indicate the start and stop of bladder infusions. Stimulation: frequency: 14 Hz, intensity, 0.7 to 8 V. Infusion rate: 30 mL/min. NS, normal saline; AA, acetic acid; SNM, sacral nerve stimulation.
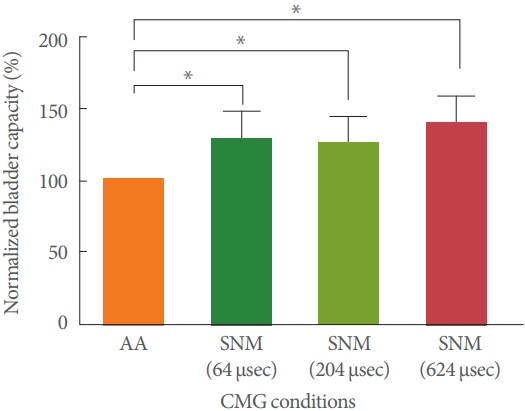
Summarized capacity results from 7 pigs during sacral neuromodulation treatment with different pulse widths. During acetic acid infusion, sacral neuromodulation at 64 µsec, 204 µsec, and 624 µsec all significantly increased the bladder capacity compared with the acetic acid level (*P<0.05). Stimulation: frequency, 14 Hz; intensity, 0.7 to 8 V. AA, acetic acid; SNM, sacral nerve stimulation; CMG, cystometrogram. *Statistically significant difference.
Intensity Thresholds From T Visuals for Different Pulse Widths
All pigs showed perianal and/or tail movements when the stimulator was turned on. The actual intensity threshold was 0.7 to 8 V. The mean intensity thresholds for a pulse width of 64 μsec, 204 μsec, and 624 μsec were 5.64±0.76 V, 3.11±0.48 V and 2.52±0.49 V, respectively. T visuals for pulse widths of 64 μsec were significantly larger than the other 2 T visuals for pulse widths of 204 μsec and 624 μsec (P<0.05) (Fig. 7). No significant differences were found among the T visuals for pulse widths of 204 μsec or 624 μsec (P>0.05).
DISCUSSION
In this study, we adopted a model from the current clinical practice of electrode placement in human SNM and the Sacral-Stim system implanted through the S3 sacral foramen in pigs [10,13]. From the result that AA induced overactivity and reduced bladder capacity compared with the NS control levels (Figs. 4, 6), we can see that we successfully instilled AA into the pig bladders. We think that the damage of AA to the bladder mucosa is permanent.
We chose 14 Hz because it is recommended in clinical practice [14]. The intensity threshold for inducing perianal and/or tail movement was determined by gradually increasing the stimulation intensity, because motor responses are markers of placement success in clinical practice. The sacral nerve was activated by electrical stimulation over a range of pulse widths so we could compare pulse width response curves. In our study, we found that SNM at 64 μsec, 204 μsec, and 624 μsec pulse widths all significantly increased bladder capacity during AA infusion. However, no significant differences were observed in the results obtained using 64 μsec, 204 μsec, or 624 μsec pulse widths (Figs. 5, 6). In the second part of our experiment, we compared the values of T visuals corresponding to different pulse widths and found that T visuals for pulse widths of 64 μsec were significantly larger than the other 2 T visuals for pulse widths of 204 μsec and 624 μsec (P<0.05), which is consistent with Suxin’s research [15]. In their studies, T visuals for shorter pulse widths were larger, but the rheobase was about 0.4 to 0.7 V, and maximal thresholds with the minimal pulse widths were as high as 2 to 4 V, which was lower than our T visual. This may be due to the different animal models used and the different position of the electrode inserted.
Grill and Mortimer’s theoretical study suggested that varying the stimulus current pulse width would be effective in achieving selective recruitment of motor units based on the different electrical recruitment properties for myelinated nerve fibers of varying sizes [16]. It has been reported that the average recruited fiber diameter decreases with increasing pulse width and the distribution for recruited nerve fibers remains the same for pulse widths of 300 μsec to 1 msec [11]. This may explain why no significant differences were found among the T visuals for pulse widths of 204 μsec and 624 μsec.
Mohamed et al. [2] reported that sacral nerve stimulation may inhibit bladder overactivity through several mechanisms, including the inhibition of bladder afferent pathways of the micturition reflexes and/or activation of the hypogastric sympathetic pathways. It has been reported that, under physiological conditions, bladder distention by NS infusion primarily activates nonnociceptive bladder Aδ-afferent fibers. However, under pathological conditions, bladder irritation induced by AA infusion activates nociceptive C-afferent fibers, which induce a spinal micturition reflex [17]. It is assumed that the inhibitory effect of SNM on bladder activity is partially due to the activation of the large-diameter pudendal afferent nerves in the sacral dorsal roots [18].
Su et al. [10] showed that the optimal pulse widths s of the SNM were about 40 to 50 μsec in sheep models which are much shorter than the 210 μsec typically used in clinical studies. At fixed 10-Hz motor threshold intensity, shorter pulse widths of nerve stimulation are equally effective in attenuation of the frequency of bladder contractions as the longer pulse widths [15]. Shorter pulse width stimulation may increase the window and reduce discomfort due to higher nerve fiber selectivity than the 0.21 msec pulse width widely used clinically.
Generally, a response threshold in the range of 0.5 to 2.0 V is preferred in human testing to ensure adequate space between the nerve and the electrode and to maintain patient comfort during stimulation [19]. Because the T visual for pulse widths of 64 μsec was significantly higher than that of the other two groups, and a T visual of 64 μsec was as high as 5.64±0.76 V, there was no significant difference in the increase of bladder capacity; the minimum pulse width (64 μsec) may not be suitable for clinical use. To minimize energy consumption and maintain patient comfort during stimulation, 204 μsec may be an appropriate pulse width for SNM because no significant differences were found among the T visuals for pulse widths of 204 μsec and 624 μsec.
These results indicate that different pulse widths may play a role in inhibiting bladder overactivity. In testing stage, we can try more pulse widths especially between 64 μsec and 210 μsec. If the T visuals are the same, we can use shorter pulse widths to minimize energy consumption from the implantable neurostimulator battery.
This study has some limitations, and some issues remain to be studied in the future. First, there were only three groups of different pulse widths; There was really a wide spectrum of pulse width from 64–624 μsec. In the first 2 pigs, we carried out 5 groups of pulse width tests (64, 204, 344, 484, and 624 μsec). However, the CMGs were performed many times to achieve a balanced bladder capacity and the bladder function needed time to recover. the pigs cannot stand if 5 groups of pulse width tests were carried out. We found the shortest and longest pulses were 64 μsec and 624 μsec respectively due to machine limitations. 210 μsec is commonly used for human SNM; thus, we chose 64 μsec, 204 μsec, and 624 μsec to identify the appropriate pulse width for SNM. After our experiments we found that more stimulation pulse widths, especially of 64 μsec to 300 μsec, need to be investigated in the future. Second, only objective motor responses, but not sensory behavior to SNM, was evaluated in pigs in this study, though some experts believe that a positive motor response is more predictive than a sensory response in successful treatment [20]. Both sensory responses and motor responses are desired to achieve optimal lead placement intraoperatively. But it is hard to check sensory response in anesthetized pigs. Maybe we could correlate sensory response with motor response in humans in the future; Third, the level of the anesthetic varies from one animal to another one. Considering the effect of anesthesia on the bladder function, we did not use the muscle relaxants in our experiment. The anesthetics drugs we used in this experiment had very little effect on bladder function. Though we have tried our best to minimize the impact of anesthesia on the data, the anesthesia has a certain effect on the results of the experiment. Thus, further research in the clinic is needed. Fourth, SNM was applied acutely in our study, while inpatient stimulations are delivered long term. It is necessary to examine the effects of chronic stimulation on the sacral nerves in the future.
In conclusion, this study indicated that different pulse widths may play a role in inhibiting bladder overactivity. It is not yet certain which pulse widths are best to increase bladder capacity compared with the AA level; however, to minimize energy consumption and maintain patient comfort during stimulation, 204 μsec may be an appropriate pulse width for SNM.
Notes
Research Ethics
The Animal Care and Use Committee at Capital Medical University approved all protocols involving the use of animals in this study (AEEI-2016-113).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION STATEMENT
·Full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis: HC, LL, ZW, YW, LZ
·Study concept and design: HC, LL, YW
·Acquisition of data: HC, LL, YW, LZ
·Analysis and interpretation of data: HC, LL, YW, LZ, ZW
·Drafting of the manuscript: HC, LL
·Critical revision of the manuscript for important intellectual content: HC, LL, ZW
·Statistical analysis: HC, ZW, LZ
·Obtained funding: LL
·Administrative, technical, or material support: GF, GC, LL
·Study supervision: LL, GF, GC