|
 |


- Search
| Int Neurourol J > Volume 25(3); 2021 > Article |
|
ABSTRACT
Purpose
In this study, a urinary management system was established to collect and analyze urinary time and interval data detected through patient-worn smart bands, and the results of the analysis were shown through a web-based visualization to enable monitoring and appropriate feedback for urological patients.
Methods
We designed a device that can recognize urination time and spacing based on patient-specific posture and consistent posture changes, and we built a urination patient management system based on this device. The order of body movements during urination was consistent in terms of time characteristics; therefore, sequential data were analyzed and urinary activity was recognized using repeated neural networks and long-term short-term memory systems. The results were implemented as a web (HTML5) service program, enabling visual support for clinical diagnostic assistance.
Results
Experiments were conducted to evaluate the performance of the proposed recognition techniques. The effectiveness of smart band monitoring urination was evaluated in 30 men (average age, 28.73 years; range, 26–34 years) without urination problems. The entire experiment lasted a total of 3 days. The final accuracy of the algorithm was calculated based on urological clinical guidelines. This experiment showed a high average accuracy of 95.8%, demonstrating the soundness of the proposed algorithm.
Conclusions
This urinary activity management system showed high accuracy and was applied in a clinical environment to characterize patients’ urinary patterns. As wearable devices are developed and generalized, algorithms capable of detecting certain sequential body motor patterns that reflect certain physiological behaviors can be a new methodology for studying human physiological behaviors. It is also thought that these systems will have a significant impact on diagnostic assistance for clinicians.
Hospitals offer a variety of tools to help clinicians care for patients receiving diuretics, including urination charts. Although urination charts are described in textbooks as one of the most important diagnostic tools for urination [1-3], these blank charts can contain inaccurate data because they are written by the patient, similar to how journal entries are written. Even if patients are well trained, as is the case in clinical studies, many studies have found that the recorded data may be inaccurate [4-6]. Furthermore, because many variables are involved in the interpretation of these records (usually because patients’ abilities to record their activities are different), it is difficult to use urinary charts to obtain accurate measurements of urinary activity. If these problems could be solved, it would be possible to provide more systematic and efficient care for patients receiving diuretics. Under these circumstances, it is increasingly necessary to come up with a plan to apply information technology to a recording system of urinary activity. Accurate detection techniques using urination monitoring capabilities can systematically and efficiently manage patient urination by duplicating the functions of urination logs. To this end, a management system was developed to recognize patients’ urinary activity by collecting and analyzing information on movements detected by smart bands (magnetic and distance information) worn by patients.
Various methods and learning algorithms for motion recognition have been proposed. Most studies have used static algorithms such as artificial neural networks [7-11] and K-means clustering [12-14], or dynamic time warping [15] in combination with algorithms. However, a time series algorithm should be used to predict or classify dynamically changing time series data. Typical time series algorithms include dynamic Bayesian networks [16], hidden Markov models (HMMs) [17], and recurrent neural networks (RNNs) [18]. The HMM and RNN methods have been widely used for time series data. However, HMMs are not appropriate for learning sequential data because each step is only influenced by the previous one.
In this study, we propose an algorithm for recognizing the movements involved in urination by analyzing data from acceleration signals and gyro signals collected from smart bands. To do so, we developed an analytical technique that enables high accuracy, while solving the limitations of existing studies. Thus, we applied an RNN-based long short-term memory (LSTM) [19,20] method for urination recognition. In addition, functions were developed to show and manage patient urinary activity history information to provide diagnostic assistance for t clinicians. This was integrated into the overall system-level functionality to efficiently manage urological patients. A conceptual diagram of the urination management system is shown in Fig. 1.
Participants’ average age was 28.73 years (range, 26–34 years), and the study was limited to patients with no signs of urination disorders. Users completed a 3-day urination log and wore a smart band to monitor the number of urinations. The smart band used in this study recognized urinary activity by combining gyro sensor information from male patients with distance information (i.e., height information relative to the ground). In this study, an improved method of LSTM-based RNN was applied based on changes in patients’ posture to increase the accuracy of urinary research. In conventional studies [21], complex data are classified simultaneously, so this system has been used to solve problems with techniques that are difficult to analyze in multiple dimensions. This method determines the class to which newly entered signal information belongs based on learned boundaries, such as characterization and classification of gyro sensor information in male patients and distance information (i.e., the height from the ground). A paper urinary diary was reviewed by 2 urologists and compared to the data reported by the smart band.
We also developed a system that enables efficient patient management by gathering and managing the history information of urological patients for clinical diagnostic assistance. This system visualizes the results of urinary activity recognition, enabling appropriate feedback for urological patients.
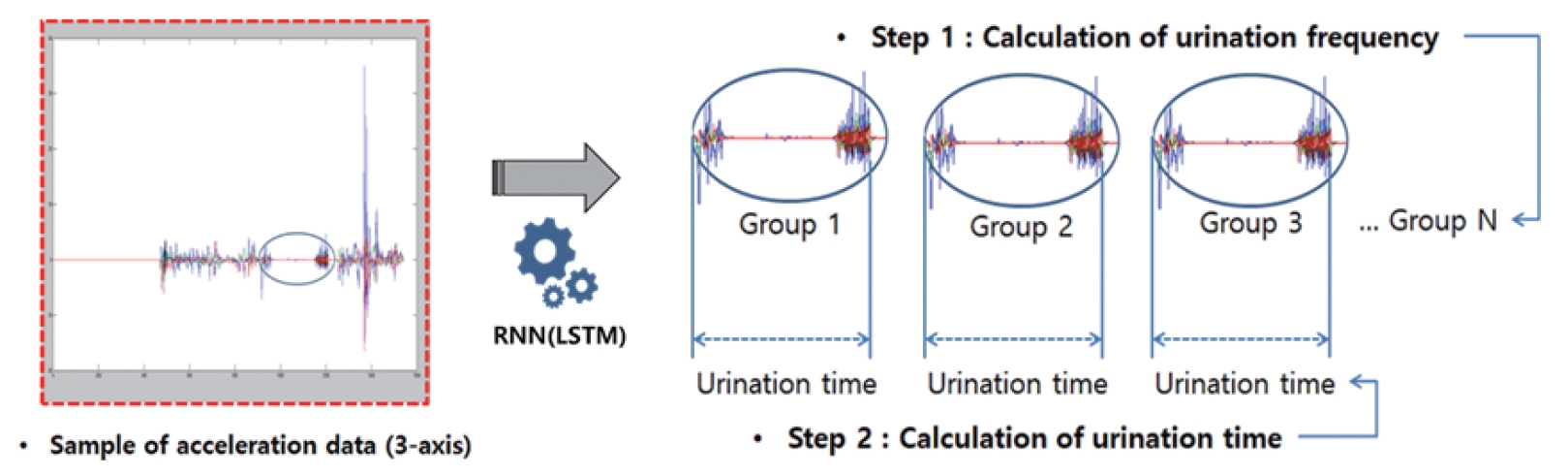
RNNs are a deep-learning method that is effective in learning sequences based on structures with repeated weights in hidden layers; RNNs recognize regular patterns of data in the same way as convolutional neural networks (CNNs) [22]. To address the limitations of existing RNNs, LSTM was applied. The LSTM algorithm is used to troubleshoot zero-gradient problems, also known as decimation-gradient problems. The LSTM is a weight structure designed to deliver gradients throughout the back-propagation process. An LSTM unit consists of cells with multiple gates attached and has the ability to store, retrieve, and maintain cell information. This feature addresses the extinction-gradient problem observed in RNNs and makes it easier to remember information from a long time ago. The LSTM addresses the extinction-gradient problem of the RNN by applying fixed weight values of 3 gates and cells. These LSTM-based RNNs were applied to handle urinary activity (frequency, time) recognition. Fig. 2 illustrates the concept of automatically recognizing the patient’s urinary activities by applying LSTM-based RNNs.
An important part of the management of patients’ urinary activity is patient feedback. To this end, a web-based (HTML5) urinary activity management system was developed, which allowed the systematic and cumulative management of patients’ urinary activity. The system construction was largely carried out in 3 stages: DB development, Backend development, and Client development. The Client optimized the switching speed between utilization programs through the Angular JS framework, the Backend was configured using Firebase, and DB development was stored in a document method based on NoSQL. We developed an integrated patient management system including a history viewer function for collected urinary activity data, the capability of automatically providing analytical information related to urinary timing by recognizing it through an LSTM-based RNN applied to collected data, and the ability for clinicians to provide feedback in an efficient manner, thereby providing clinical support. Fig. 3 illustrates the implementation screens of the intelligent patient management system.
The performance of the urination recognition technology was analyzed statistically using a confusion matrix. A total of 30 patients were selected, and the performance of the algorithm was evaluated based on data collected from smart bands (acceleration, inclination angle) over 60 days. The final accuracy of the algorithm was calculated based on clinical guidelines used by urologists. The proposed experimental method was divided into 2 main steps for recognizing urinary activity, and urinary time was calculated in the group of patients wherein urinary activity was recognized.
Information on acceleration and inclination angles was collected at frequencies between 12 and 13 Hz, and coordinates of the x-, y-, and z-axes were stored on the smartphone as time series data. The data were reformatted in XML (extensible markup language) and divided into a 3:7 ratio of learning and test data. The feature information we tried to extract included 3 steps: a forward motion to prepare for urination, a backward motion to clean oneself after urination, and urination step. The final urination recognition results were provided considering these 3 levels of information on acceleration and the inclination angle. The highest probability distribution value of the sequence data was selected as the output of the network. The output nodes were labeled for each task and learned using back-propagation algorithms, where x, y, and z represented the structure in which the accelerometer and gyro sensor signal data were entered. This comprised the process of calculating node continuity and the state of the current point at time (t) and the next point at time (t+1). Processing the target network involved 2 main steps. From phase I, the final urination phase was determined by comparing the perceived urination phase in the network with the perceived urination phase in the second-stage gyro data through the input of accelerometer data.
After the experiment was carried out, a confusion matrix (Table 1) for the proposed method and the existing method was calculated, and the accuracy was shown through actual differences in terms of seconds (Table 2) and receiver operating characteristic (ROC) curves (Fig. 4). Each number in Table 1 denotes the actual number of tests, with a total of 60 confusion tests. The numbers displayed in Table 2 have units in seconds; this table represents the average absolute values of time differences obtained through testing in 60 cases. The results showed an average accuracy of 95.6% in recognizing urinary activity, confirming the validity of urinary activity recognition. The ROC curve for the system proposed herein is shown in Fig. 4 along with each comparison method.
This paper proposes a method to assist in making an efficient clinical diagnosis through the establishment of an automatic urinary management system for urological patients. To this end, an LSTM-based RNN method was used to recognize patients’ urinary activity, and the results were visualized through a web-based program to assist clinicians’ diagnosis.
Existing classification methods are capable of recognizing the number of urination events, but it is difficult to analyze urination time using these methods due to the loss of location information when converting spatial data. Instead, the RNN method using the LSTM structure is appropriate for this goal because it analyzes the urine collection time and collects data continuously. The calculation of urination time is processed by identifying positional information over time in the forward and backward movements involved in urination. Processing is conducted through the recognition method of the RNN structure. Specifically, the proposed urination recognition technology collects acceleration and inclination angle information from smart bands and applies an LSTM structure-based RNN to derive the final urination frequency and time.
The performance of the proposed system for urinary activity recognition was evaluated using a study population of 30 actual urological patients who collected data for 60 days. The results showed an average accuracy of 95.6% in recognizing urinary activity, confirming the validity of urinary activity recognition. In addition, the urination time can be calculated after urinary activity is recognized, which will ultimately allow a comprehensive evaluation of urination in patients with urinary dysfunction. On this basis, the ultimate goal is to consider the personal characteristics of individual patients when calculating the doses of medications affecting urination. Some inaccurate results in recognizing urinary activity resulted from errors in the calculation of weights for accelerometers and gradient data. For urinary activity time measurements, the recognition rate of LSTM was found to be lower than that of comparable methods. However, the neural network was composed of random initial weights, so the average recognition accuracy was still high. To improve recognition accuracy, we plan to utilize Dempster-Shaper theory [23] or bidirectional LSTM [24], wherein 2 hidden nodes are placed in the forward and backward directions on RNN input and output nodes. In addition, if the amount and quality of data are ensured in the future, a CNN model can be applied to time series data; future research should also consider analyzing big data and developing CNN and RNN fusion deep-learning models.
In conclusion, recognizing urinary activity and providing feedback through a urinary patient management system makes it possible to monitor a patient’s actual urinary patterns. The system described in this study can be a useful option for diagnostic assistance.
NOTES
Fund/Grant Support
This work was supported by research fund of Chungnam National University Hospital.
Research Ethics
This research was approved by the Institutional Review Board of Gachon University Gil Medical Center (approval number: GDIRB2017-096).
Conflict of Interest
KHK, the corresponding author of this article, is the editor-in-chief of INJ. However, they played no role whatsoever in the editorial evaluation of this article or the decision to publish it. Except for that, no potential conflict of interest relevant to this article was reported.
REFERENCES
1. Klevmark B. Natural pressure-volume curves and conventional cystometry. Scand J Urol Nephrol Suppl 1999;201:1-4. 
2. McGuire EJ, Cespedes RD, Cross CA, O’Connell HE. Videourodynamic studies. Urol Clin North Am 1996;23:309-21. PMID: 8659029


3. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 2002;21:167-78. PMID: 11857671


4. Jarvis GJ, Hall S, Stamp S, Millar DR, Johnson A. An assessment of urodynamic examination in incontinent women. Br J Obstet Gynaecol 1980;87:893-6. PMID: 7426486


5. Webb RJ, Fawcett PR, Neal DE. Electromyographic abnormalities in the urethral and anal sphincters of women with idiopathic retention of urine. Br J Urol 1992;70:22-5. 
6. Kim SH, Oh SA, Oh SJ. Voiding diary might serve as a useful tool to understand differences between bladder pain syndrome/interstitial cystitis and overactive bladder. Int J Urol 2014;21:179-83. PMID: 23841824


7. Haykin S. Neural networks: a comprehensive foundation. New York: MacMillan; 1994.
8. Karmonik C, Boone T, Khavari R. Data-driven machine-learning quantifies differences in the voiding initiation network in neurogenic voiding dysfunction in women with multiple sclerosis. Int Neurourol J 2019;23:195-204. PMID: 31607098



9. Kim JW, Kim SJ, Park JM, Na YG, Kim KH. Past, present, and future in the study of neural control of the lower urinary tract. Int Neurourol J 2020;24:191-9. PMID: 33017890



10. Nikkola J, Holm A, Seppänen M, Joutsi T, Rauhala E, Kaipia A. Repetitive transcranial magnetic stimulation for chronic prostatitis/chronic pelvic pain syndrome: a prospective pilot study. Int Neurourol J 2020;24:144-9. PMID: 32615676




11. Prabhakar AT, Iqbal Ahmed AS, Vijayakrishnan Nair A, Mathew V, Aaron S, Sivadasan A, et al. Neural correlates of urinary retention in lateral medullary infarction. Int Neurourol J 2019;23:205-10. PMID: 31607099



12. Fraley C, Raftery AE. Model-based clustering, discriminant analysis, and density estimation. J Am Stat Assoc 2002;97:611-31. 
13. Moon JU, Cho KO. Current pharmacologic strategies for treatment of intractable epilepsy in children. Int Neurourol J 2021;25(Suppl 1):S8-18. PMID: 34053206



14. Baser A, Eliaçık S, Baykam MM, Tan FU. Clinical manifestations of overactive bladder with migraine as a comorbidity: a prospective cross-sectional study. Int Neurourol J 2020;24:375-81. PMID: 33401359



15. Berndt DJ, Clifford J. Using dynamic time warping to find patterns in time series. Proceeding AAAIWS’94 Proceedings of the 3rd International Conference on Knowledge Discovery and Data Mining. 1994 Jul 31-Aug 1; Seattle (WA), USA: 1994. 359-70.
16. Murphy KP. Dynamic bayesian networks: representation, inference and learning [thesis]. University of California, Berkeley; Berkeley (CA): 2002.
17. Sonnhammer EL, von Heijne G, Krogh A. A hidden Markov model for predicting transmembrane helices in protein sequences. Proc Int Conf Intell Syst Mol Biol 1998;6:175-82. PMID: 9783223

19. Hochreiter S, Schmidhuber J. Long short-term memory. Neural Comput 1997;9:1735-80. PMID: 9377276


20. Whangbo TK, Eun SJ, Jung EY, Park DK, Kim SJ, Kim CH, et al. Personalized urination activity recognition based on a recurrent neural network using smart band. Int Neurourol J 2018;22(Suppl 2):S91-100. PMID: 30068071



21. Eun SJ, Whangbo TK, Park DK, Kim KH. Development of personalized urination recognition technology using smart bands. Int Neurourol J 2017;21(Suppl 1):S76-83. PMID: 28446018



22. Simard PY, Steinkraus D, Platt JC. Development of personalized urination recognition technology using smart bands. Proceedings of the Seventh International Conference on Document Analysis and Recognition (ICDAR 2003). 2003 Aug 3-6; Washington, DC, USA: Piscataway (NJ): Institute of Electrical and Electronics Engineers; 2003. 958-62.
23. Valente F, Hermansky H. Combination of acoustic classifiers based on Dempster-Shafer theory of evidence. 2007 IEEE International Conference on Acoustics, Speech and Signal Processing - ICASSP. 2007 Apr 15-20; Honolulu (HI), USA: 2007. IV-1129-32. 
24. Liwicki M, Graves A, Bunke H, Schmidhuber J. A novel approach to on-line handwriting recognition based on bidirectional long short-term memory networks. ICDAR 2007 Proceedings of the Ninth International Conference on Document Analysis and Recognition. 2007 Sep 23-26; Washington, DC: IEEE Computer Society; 2007.
25. Vapnik V, Mukherjee S. Support vector method for multivariate density estimation. Adv Neural Inf Process Syst 2000;659-65.
Fig. 1.
Conceptual diagram of the urination management system. Adapted from Whangbo et al. Int Neurourol J 2018;22(Suppl 2):S91-100 [20].
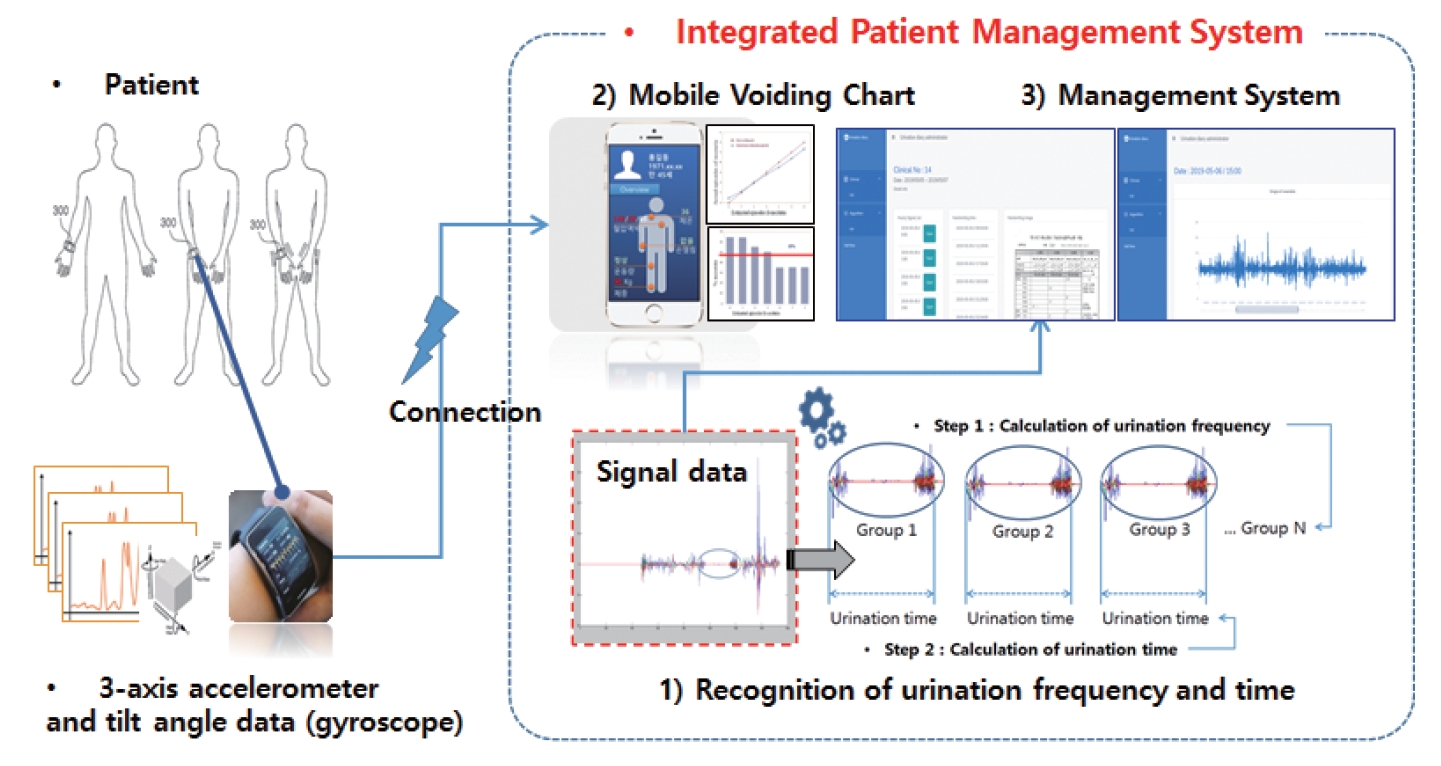
Fig. 3.
Implementation screens of the intelligent patient management system. RNN, recurrent neural network; LSTM, long short-term memory.
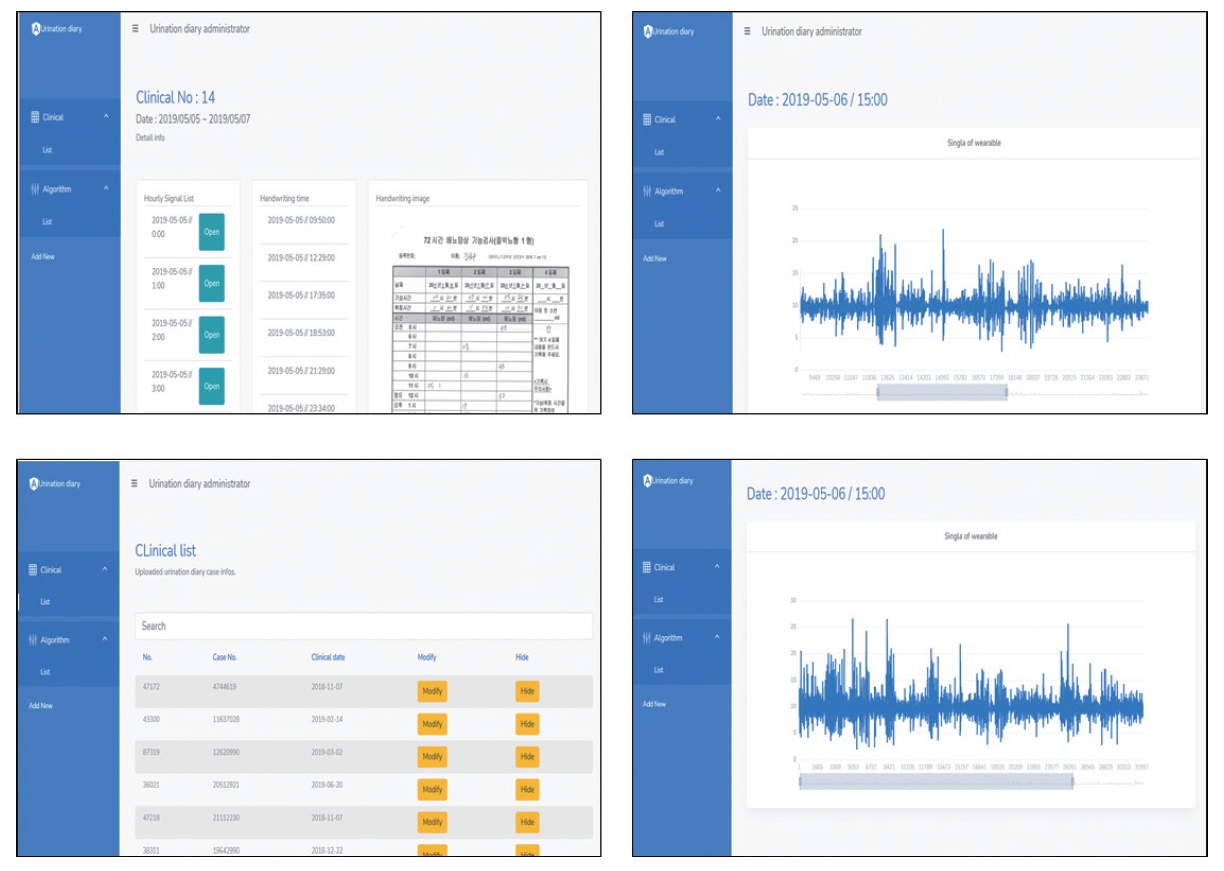
Fig. 4.
Receiver operating characteristic comparison of each methods. HMM, hidden Markov model; SVM, support vector machine.
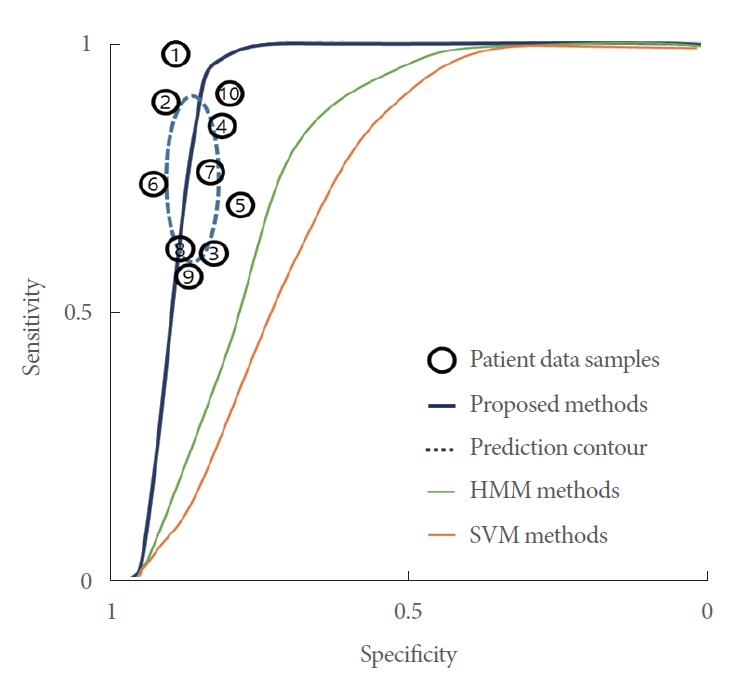
Table 1.
Comparison of the proposed method with other existing methods
| Confusion matrix | Proposed method | HMM-based [17] | SVM-based [25] |
|---|---|---|---|
| True positive | 55 | 42 | 37 |
| False positive | 5 | 18 | 23 |
| True negative | 56 | 50 | 42 |
| False negative | 4 | 10 | 18 |
Table 2.
Accuracy of urinary activity time (sec) measurements
| Participant (1–30) | Proposed method | HMM-based [17] | SVM-based [25] |
|---|---|---|---|
| 1 | 3.21 | 4.48 | 8.25 |
| 2 | 2.89 | 5.26 | 11.43 |
| 3 | 3.52 | 7.36 | 8.68 |
| 4 | 1.49 | 3.25 | 9.57 |
| 5 | 6.89 | 6.54 | 7.45 |
| 6 | 5.16 | 7.87 | 11.38 |
| 7 | 2.6 | 5.34 | 9.45 |
| 8 | 3.25 | 4.64 | 8.32 |
| 9 | 3.77 | 8.68 | 10.18 |
| 10 | 2.81 | 5.76 | 9.24 |
| ... | ... | ... | ... |
| Matched | 22 | 5 | 3 |