Reduction of Bladder Capacity Under Anesthesia Following Multiple Recurrences and Repeated Surgeries of Hunner Lesions in Patients With Interstitial Cystitis
Article information
Abstract
Purpose
To investigate the influence of multiple recurrences and repeated surgeries of Hunner lesions on bladder capacity under general anesthesia in patients with interstitial cystitis (IC).
Methods
We retrospectively reviewed the clinical records of Hunner-type IC (HIC) patients who underwent transurethral fulguration or resection of Hunner lesions combined with hydrodistension by a single surgeon between 2011 and 2020. Recurrence was defined as reappearance of uncontrolled urinary symptoms in association with new Hunner lesions identified by cystoscopy. Recurrent Hunner lesions were then treated by transurethral surgeries. The recurrence-free rate, potential predictive factors of recurrence, and changes in bladder capacity under anesthesia were examined at each surgical procedure.
Results
A total of 92 surgeries were performed in 47 HIC patients, 23 (49%) of whom required multiple procedures (range, 1–5 times). The mean recurrence-free time after the first surgery was 21.7 months. The recurrence-free rate was 53% at 24 months, and decreased to 32% at 48 months. There were no significant differences in age, sex, bladder capacity under anesthesia at the first surgery, duration from symptom onset to the first surgery, O’Leary-Sant questionnaire including symptom and problem indexes, visual analogue scale pain score, and the number of comorbidities between the cases with or without recurrence. Bladder capacity under anesthesia was gradually decreased as the number of surgeries was increased, and bladder capacity at the fourth procedure was significantly decreased to 80% of the capacity at the first surgery.
Conclusions
These results suggest that multiple recurrences and repeated surgeries of Hunner lesions result in a reduction of bladder capacity under anesthesia in HIC patients although no predictive factors for recurrence of Hunner lesions were detected.
INTRODUCTION
The East Asian guideline defines interstitial cystitis/bladder pain syndrome (IC/BPS) as a condition with chronic pelvic pain, pressure, or discomfort perceived to be related to the urinary bladder accompanied by other urinary symptoms, such as persistent urge to void or urinary frequency in the absence of confusable diseases [1]. The current concept is that patients diagnosed with IC/BPS display at least 2 distinct phenotypes: a bladder-centric IC phenotype with Hunner lesions (HIC), in which pain symptom is rather confined to the bladder, and a systemic syndrome phenotype (BPS) where lower urinary tract symptoms and pain are more overlapped with systemic symptoms and other syndromes such as irritable bowel syndrome and depression [2].
The extent of Hunner lesions on the bladder surface has been reported to be associated with urinary symptom severity and reduced bladder capacity [3]. Transurethral fulguration or resection of Hunner lesions combined with hydrodistension is recommended as the third-line treatment for HIC patients in clinical guidelines [4], which can alleviate bladder pain during the storage phase and increase bladder capacity compared with transurethral fulguration or resection alone [5]. Ko et al. [6] have also demonstrated that there were no significantly differences in recurrence-free time between transurethral fulguration and transurethral resection of Hunner lesions using a prospective randomized clinical trial.
It has recently been reported that IC/BPS patients with low bladder capacity less than 400 mL under general anesthesia had histological evidence of significantly more acute and chronic inflammation compared with those with non-low bladder capacity, supporting that the low anesthetic bladder capacity could be a marker of a bladder-centric IC/BPS phenotype [7]. Peeker and Fall [8] have also reported that significant differences between anesthetic bladder capacity of HIC and non-Hunner BPS patients (468 and 747 mL, respectively) were larger compared with functional bladder capacity (199 and 248 mL, respectively), suggesting that anesthetic bladder capacity is more appropriate to use as a marker to identify 2 distinct IC/BPS phenotypes compared with functional bladder capacity.
The influence of multiple recurrences and repeated surgeries on anesthetic bladder capacity in HIC patients have remained controversial. Chennamsetty et al. [9] have reported that a total of 214 surgeries were performed in 76 HIC patients, 51 (67%) of whom required multiple procedures with the mean number of 3.0 surgeries (range, 1–11 times), and that the repeated surgeries did not significantly reduce mean anesthetic bladder capacity (initial, 439 mL; final, 422 mL) although the number of surgeries was negatively correlated with the changes in anesthetic bladder capacity. Tomoe and Yamashita [10] have also reported that a total of 109 surgeries were performed in 44 HIC patients, all of whom required the second surgery, and 21 (48%) of whom underwent the third surgery. There were no significant changes in mean functional bladder capacity measured by a 4-day frequency volume chart after each surgery (first, 173 mL; second, 166 mL; third, 168 mL) although anesthetic bladder capacity at the third surgery (349 mL) was significantly reduced compared with the capacity at the first surgery (440 mL). Furthermore, Peeker et al. [11] have reported that a total of 259 surgeries were performed in 103 HIC patients and that 22 (21%) of them required multiple procedures (range, 1–16 times) and developed the small capacity bladder. Based on these findings, this study was designed to investigate the influence of multiple recurrences and repeated surgeries on anesthetic bladder capacity in HIC patients because bladder capacity reduction is an important contributing factor to high intravesical pressure, resulting in vesicoureteral reflux and renal failure in HIC patients.
MATERIALS AND METHODS
We retrospectively reviewed the clinical records of HIC patients treated at the Jikei University Hospital between 2011 and 2020 after obtaining the institutional ethics approval (No. 8735). We included only patients who underwent transurethral fulguration or resection of Hunner lesions combined with hydrodistension performed by a single surgeon (AF) during this period. O’Leary-Sant questionnaire including symptom and problem indexes (O’Leary-Sant symptom index [OSSI] and O’Leary-Sant problem index [OSPI]) and visual analogue scale (VAS) pain score were completed to evaluate urinary symptom severity before each surgical treatment.
The surgical procedure was performed when Hunner lesions were identified during cystoscopy in patients who exhibited uncontrolled urinary symptoms. Under general anesthesia, Hunner lesions were at first detected in the bladder when the bladder was slightly filled with saline under cystoscopic observation. The bladder was then distended with saline through a cystoscopic port until bladder pressure reached to 80 cm H2O or mucosal cracking, and the pressure was then maintained for 5 minutes. If bladder capacity under anesthesia was estimated based on the volume infused during hydrodistension. After hydrodistension, biopsies were performed at all suspicious areas of Hunner lesions to rule out confusable diseases such as malignancy and tuberculosis, and Hunner lesions were then completely fulgurated or resected with a small rim of the normal mucosa being kept intact at the lesion’s outer margin. Also, attempts were made to avoid fulguration or resection of the grossly normal mucosa during the procedure.
In all patients, a postoperative follow-up visit was recommended within 2 weeks after the surgical procedure. Beyond the first postoperative visit, the patients were followed up every 2 months or at the earlier time point when the therapeutic benefit of surgical procedures began to decrease. Cystoscopy along with assessment of OSSI, OSPI, and VAS pain score was performed every 6 months for 5 years by the same surgeon. The recurrence of Hunner lesions was defined as an identification of new Hunner lesions by cystoscopy in HIC patients who had reappearance of uncontrolled urinary symptoms after the surgical procedure. To evaluate the predictive factors of Hunner lesion recurrence, we examined the association with clinical features including age, sex, bladder capacity under anesthesia at the first surgery, duration from the symptom onset to the first surgery, OSSI, OSPI, VAS pain score, and the number of comorbidities such as lumber spinal stenosis, Sjogren syndrome and depression between the cases with or without recurrence. In addition, changes in anesthetic bladder capacity at each repeated procedure as well as intersurgical intervals were examined.
All data were represented as mean values±standard deviation of the mean. Statistical analysis software (Prism, GraphPad Software, San Diego, CA, USA) was used to perform the data analysis. Recurrence-free time after the first surgery was evaluated using Kaplan-Meier analysis. Significant differences in age, bladder capacity under anesthesia at the first surgery, duration from the symptom onset to the first surgery, OSSI, OSPI, and VAS pain score were analyzed using Mann-Whitney U-test whereas differences in the sex and the number of comorbidities were detected by chi-square test. In addition, changes in the intersurgical intervals, bladder capacity under anesthesia at each procedure with its ratio compared with the capacity at the first surgery were examined using Kruskal-Wallis test followed by Dunn multiple comparison test.
RESULTS
In total, 8 males (17%) and 39 females (83%) were included in this study. The mean age of the entire cohort was 59.0 years. All 47 HIC patients met the National Institute of Diabetes and Digestive and Kidney Diseases criteria [12]. The mean duration from the symptom onset to the first surgery was 23.7 months. Before the first procedure, all patients were treated with oral medications, which did not improve their symptoms, and mean OSSI, OSPI, and VAS pain scores were 14.6, 12.6, and 8.5, respectively.
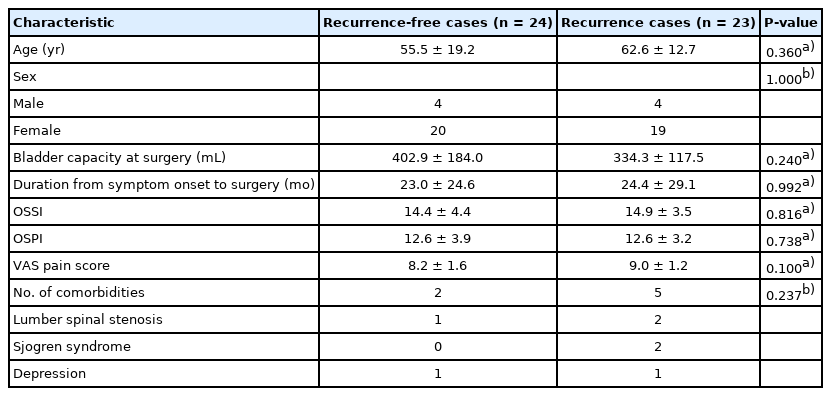
A total of 92 surgeries were performed in 47 HIC patients, 23 (49%) of whom required multiple surgical procedures for recurrent Hunner lesions (range, 1–5 times). There were no significant differences in age, sex, anesthetic bladder capacity at the first surgery, duration from the symptom onset to the first surgery, OSSI, OSPI, VAS pain score, or the number of comorbidities including lumber spinal stenosis, Sjogren syndrome, or depression between 2 patient cohorts with or without recurrence (Table 1).
The mean recurrence-free time after the first procedure was 21.7 months. The recurrence-free rate was 80% at 12 months, 53% at 24 months, 43% at 36 months, 32% at 48 months, and 26% at 60 months (Fig. 1).

The recurrence-free rate of Hunner lesions after transurethral fulguration or resection combined with hydrodistension. The mean recurrence-free time after the first procedure was 21.7 months.
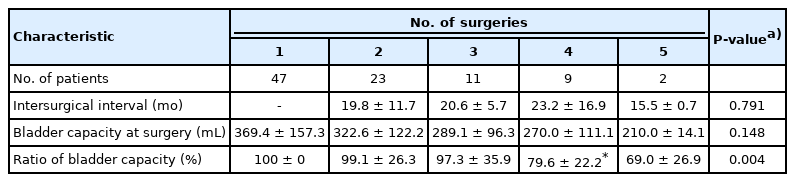
The results of the intersurgical interval, anesthetic bladder capacity at each surgery, and its ratio to the first procedure capacity were shown in Table 2. The mean intersurgical interval was 20.5 months without significant differences among intersurgical intervals at any time points of surgical procedures. Bladder capacity under anesthesia at each surgery was gradually decreased from 369 mL at the first procedure to 270 mL at the fourth procedure. Although there were no significant differences among bladder capacity at different time points of surgical treatments, the ratio of bladder capacity to the capacity at the first surgery was significantly decreased to 80% at the fourth surgery (Fig. 2). In addition, no patients underwent cystectomy due to small bladder capacity in this study.

Changes in bladder capacity under anesthesia at each surgery (A) and its ratio to the capacity at the first procedure (B). Bladder capacity under anesthesia at each surgery was gradually decreased although there were no significant differences in the comparison of bladder capacity at different time points of surgical procedures. Meanwhile, the ratio of bladder capacity to the capacity at the first procedure was significantly decreased to 80% at the fourth surgery. *P<0.05 vs. the first procedure.
DISCUSSION
The results of the present study indicate that, in a total of 47 HIC patients who underwent 92 surgeries, 23 (49%) of them required multiple surgical procedures for the treatment of recurrent Hunner lesions (range, 1–5 times) and that 9 (19%) of them developed a significant reduction of anesthetic bladder capacity at the fourth procedure compared with the capacity at the first surgery. These results suggest that multiple recurrences and repeated surgeries of Hunner lesions result in a reduction of bladder capacity measured under anesthesia although there has been some controversy regarding their influence on bladder capacity in HIC patients in previous studies [9-11].
Different definitions of recurrence have been reported in HIC patients who underwent transurethral fulguration or resection of Hunner lesions combined with hydrodistension. Niimi et al. [13] have defined the recurrence when additional surgery, bladder instillation therapy and/or a narcotic use for pain control were needed, and reported that the mean recurrencefree time was 28.5 months in 126 HIC patients. It has also been reported by Peeker et al. [11] that recurrence was defined as a decision of surgery to alleviate urinary symptoms and that the mean duration of symptom alleviation was 23 months in 103 HIC patients. In the present study, recurrence was defined as an identification of new Hunner lesions by cystoscopy in HIC patients with reappearance of uncontrolled urinary symptoms, and found that the mean recurrence-free time was 21.7 months. In addition, the recurrence-free rate was 80% at 12 months and 32% at 48 months, which were similar to the previous report demonstrating that the recurrence-free rate was 87% at 12 months and 43% at 48 months in 59 HIC patients, 27 (46%) of whom required multiple procedures with the mean number of 4.3 times [14].
In this study, the association of recurrence with age, sex, bladder capacity under anesthesia, duration from the symptom onset to the first surgery, OSSI, OSPI, VAS pain score, and the number of comorbidities such as lumber spinal stenosis, Sjogren syndrome, and depression was examined; however, no significant association with any of these factors was detected, in line with the previous report [3]. On the other hand, Hillelsohn et al. [14] have reported that the incidence of depression was significantly higher in HIC patients with multiple surgical procedures versus those with single procedure although there were no significant differences in age, sex, duration from the symptom onset to the first surgery, the number of Hunner lesions and irritable bowel syndrome between the 2 groups. Niimi et al. [13] have also found lumber spinal stenosis as a predictor for recurrence, but not age, sex, bladder capacity under anesthesia, OSSI, OSPI, VAS pain score, the incidence of allergy, Sjogren syndrome, irritable bowel syndrome, or history of pelvic surgery.
The mean intersurgical interval was 20.5 months in the present study, and bladder capacity under anesthesia was gradually decreased as the number of repeated surgeries was increased. Hillelsohn et al. [14] have reported that the mean number of surgeries was 4.3 and that the mean intersurgical interval was 20.3 months. It has also been reported by Chennamsetty at al. [9] that the mean number of surgical procedures was 3.0 (range, 1–11 times) and that mean intersurgical interval was 14.5 months. Furthermore, Peeker et al. [11] have divided 97 HIC patients into 4 distinct groups; group 1 (n=40): long-term good responders defined as long-term remission (3 years or more) after a maximum of 3 surgeries, group 2 (n=35): short-term good responders who still required multiple procedures, group 3 (n=8): long-term poor responders who developed the small capacity bladder in the course of more than 2 years, and group 4 (n=14): short-term poor responders who progressed rapidly into the end-stage disease within 2 years after diagnosis. They reported that bladder capacity under anesthesia was significantly lower in group 4 compared with other 3 groups. In the present study, 9 of 47 HIC patients (19%) underwent 4 times of surgeries at mean 20.5 months intervals could be classified as group 3 in the the study of Peeker et al. [11], and might develop the further reduction in bladder capacity in the longer followup period. In addition, Lee et al. [15] have discussed the causes of small capacity bladder under anesthesia and concluded that repeated coagulation or resection of Hunner lesions triggered the reduction in bladder capacity due to fibrosis in the bladder wall. However, it can be speculated that the small capacity bladder could be caused also by multiple recurrences of Hunner lesions, which are often associated with severe lymphoplasmatic infiltration and urothelial denudation [16], because group 4 of the Peeker et al. [11] developed the small capacity bladder without multiple surgical procedures. In this regard, we have previously reported that the expression of collagen in the bladder wall was significantly increased in association with significant elevation of the expression of transforming growth factor-β (TGF-β) in HIC patients compared with controls [17]. In addition, it has been reported that repeated hydrodistension procedures alone did not result in significant changes in anesthetic bladder capacity in HIC patients [18].
The present study has limitations due to the small sample size and the retrospective study design. However, our study has some strengths because a single surgeon performed all the surgeries with transurethral fulguration or resection of Hunner lesions combined with hydrodistension, which are considered to be a standard procedure for the treatment of HIC [1,11]. In addition, cystoscopy as well as the assessment of patients’ symptoms using OSSI, OSPI, and VAS pain score, were performed at each procedure by the same surgeon. Thus, the consistency in diagnosis and treatment methods was well maintained without interexaminer variability in this study.
In conclusions, the results of the present study suggest that multiple recurrences and repeated surgeries result in reduction of bladder capacity under anesthesia in HIC patients although predictive factors of recurrence after surgical treatments were not detected. The reduction of bladder capacity would be caused not only by repeated surgeries, but also by multiple recurrences of Hunner lesions because Hunner lesions can induce bladder fibrosis to reduce bladder capacity due to severe inflammation with lymphoplasmatic infiltration [16] and TGF-β upregulation [17].
Notes
Research Ethics
This study was approved by the Institutional Review Board of Jikei University Hospital (No. 8735).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION STATEMENT
·Conceptualization: AF, NY
·Data curation: AF, TI
·Formal analysis: YS, TK
·Methodology: AF
·Project administration: AF
·Visualization: AF
·Writing-original draft: AF
·Writing-review & editing: SE, NY
Acknowledgements
The authors would like to thank all the study participants. Statistical analyses were advised by Makoto Tokuda, Life Science Institute, Inc.