 |
 |


- Search
| Int Neurourol J > Volume 26(1); 2022 > Article |
|
ABSTRACT
Purpose
To identify more accurate predictors of upper urinary tract dilatation (UUTD) in neurogenic bladder (NB) children, we studied the relationship among urodynamic parameters at different bladder filling stages, detrusor leak point pressure (DLPP) and UUTD.
Methods
A total of 158 children (3‚Äď16 years) with NB were included and then divided into 2 groups according to whether their NB diagnosis was complicated with UUTD: the UUTD group (39 patients) and those without UUTD group (control group, 119 patients). The bladder filling phase was divided into 3 equal parts: the early, middle, and end filling stages. The bladder compliance (BC) and detrusor pressure (‚Ė≥Pdet) at each phase and DLPP at the end filling stage were recorded.
Results
A BC<8 mL/cm H2O both in the middle and end stages is more specific than a BC<9 mL/cm H2O in the end stage (72%, 73%, vs. 66%), and ‚Ė≥Pdet >8 cm H2O in the early stage, 20 cm H2O in the middle stage and 25 cm H2O in the end stage are more sensitive than ‚Ė≥Pdet >40 cm H2O in the end stage (82%, 85%, 85%, vs. 49%). A DLPP cutoff value of 20 cm H2O showed higher sensitivity for predicting UUTD than 40 cm H2O.
Neurogenic bladder (NB) due to spinal bifida is common in clinical practice. The upper urinary tract dilatation (UUTD) is a main cause of morbidity and mortality in children with NB [1]. Bladder compliance (BC) refers to the relationship between bladder volume and detrusor pressure and can be calculated from a cystometric pressure/volume curve. It is generally regarded as a measure of bladder stiffness or distensibility. A poor compliant bladder may increase the incidence of upper urinary tract infection and UUTD [2].
It has previously been reported that low BC is an independent predictor of UUTD [3]. The study of Kurzrock and Polse [4] revealed that BC value of <9 cm/cm H2O was an important risk factor for UUTD. Ghoniem et al. [5,6] confirmed the above viewpoints in their studies. Detrusor leak point pressure (DLPP) is also an important predictor of UUTD [5,7]. However, the literature on how to predict UUTD is still controversial. McGuire et al. [1] mentioned that approximately 70% of patients with NB and a DLPP value >40 cm H2O suffer from UUTD. Prakash et al. [7] reported that a DLPP value <40 cm H2O can also indicate UUTD, especially in the presence of vesicoureteral reflux (VUR) and an increased postvoided residual (PVR). Moreover, a recent study showed that a DLPP cutoff value of 20 cm H2O showed a higher sensitivity to predict UUTD than a cutoff value of 40 cm H2O [8]. Obviously, further studies should be performed to identify more accurate predictors of UUTD. With the advances of urodynamic study, it is possible to find more accurate urodynamic parameters to predict UUTD [9,10]. To our knowledge, there have been no reports on the relationships between BC and detrusor pressure or DLPP at different bladder filling stages and UUTD. Therefore, the purpose of this study is to evaluate the predictive value of a low BC, high detrusor pressure (‚Ė≥Pdet), and DLPP at different bladder filling stages for the diagnosis of UUTD in children with NB.
A total of 158 children with NB who visited the First Affiliated Hospital of Zhengzhou University between 2018 and 2020 were included in this study, 39 of whom had UUTD. All patients were examined by ultrasound, intravenous urography, spinal magnetic resonance imaging, and video urodynamic study (VUDS). The patients were divided into 2 groups: group 1 (UUTD group) included 39 patients with bilateral hydronephrosis and VUR (range, 3‚Äď16 years), of whom 30 had spina bifida (including cases of occult and cystic spina bifida), 6 had cystic spina bifida that was repaired, and 3 had spina bifida injury. Group 2 (control group) included 119 patients without UUTD and VUR (range, 3‚Äď16 years), of whom 93 had spina bifida (including occult and cystic spina bifida), 18 had cystic spina bifida that was repaired, and 8 had spina bifida injury. Table 1 shows all the patients‚Äô characteristics.
The results of VUDS were interpreted according to International Continence Society (ICS) and International Children‚Äôs Continence Society (ICCS) [11-14]. The urodynamic setting was a Laborie Urodynamic analyzer (Laborie Medical Technologies Inc., Mississauga, ON, Canada). A 6F double-lumen catheter was used to record the bladder pressure transurethrally. Room-temperature saline and dilute ioversol were perfused into the bladder at a rate of 10% of the expected bladder capacity (mL/min) [15]. The bladder filling endpoint was defined as the desire to void, a sensation of fullness or discomfort, or leakage around the catheter. The urodynamic parameters assessed included BC, ‚Ė≥Pdet, the maximum flow rate, PVR, and maximum cystometric capacity (MCC). The DLPP is defined as the maximum detrusor pressure needed to overcome urethral resistance was also recorded. When no leakage was observed, DLPP was replaced with the maximum Pdet at the MCC [16]. The bladder filling phase was divided into 3 equal parts, namely, the early, middle, and end filling stages. During the cystometry and pressure-flow study, recording began from the pressure (Pdet0) when the bladder was empty (V0=0 mL) to the pressure (Pdet3) when the bladder was filled to the patient‚Äôs strong desire to urinate (V3). Then, we obtained the ‚Ė≥V3 (‚Ė≥V3=V3‚ÄďV0) and ‚Ė≥Pdet3 (‚Ė≥Pdet3=Pdet3‚ÄďPdet0). In the same manner, we obtained ‚Ė≥V1 and ‚Ė≥V2 and ‚Ė≥Pdet1 and ‚Ė≥Pdet2 when the bladder volume increased to 1/3 and 2/3 of the MCC, respectively. According to the calculation formula of BC (BC=‚Ė≥V/‚Ė≥Pdet), we obtained the different BC values (BCx=‚Ė≥Vx/‚Ė≥Pdetx) in the early, middle, and end filling stages.
For the statistical analysis, t-test was used to determine the differences in BC and ‚Ė≥Pdet in different filling stages between patients with NB with and without UUTD, and P<0.05 was regarded as statistically significant. The receiver operating characteristic (ROC) curves of BC and ‚Ė≥Pdet in different filling stages were generated, the index on the point of tangency at the curve was identified, and the sensitivity (SEN) and specificity (SPE) were recorded. According to the formulas used to calculate the positive predictive value CPPV=1/[1+{1‚ÄďSPE} {1‚ÄďP}/ {SEN √óP}]) and negative predictive value (NPV =1/[1+{1‚Äď SEN}√óP/{SPE‚ÄďSPE√óP}]), (P is the probability of UUTD in all pediatric patients with NB, and its value is approximately 40%) [17], the PPV and NPV were calculated. The accuracy of BC and ‚Ė≥Pdet in different filling stages and DLPP to predict UUTD were analyzed by the area under the curve.
In the UUTD group (n=39), the pressure-volume (P-V) curves could be divided into 3 stages. The first stage (early filling stage) showed that the detrusor pressure increased slowly, the second stage (middle filling stage) revealed that the detrusor pressure increased quickly and then continued to increase slowly, and the end stage (end filling stage) showed that the detrusor pressure was at a stably high level (Fig. 1). In the middle and end filling stages, a positive correlation was found between the BC and UUTD as well as between an increase in ‚Ė≥Pdet and a high prevalence of UUTD in all 3 filling stages (Table 1).
Patients with a BC value of <8 mL/cm H2O in the middle and end stages had a slightly higher SPE than those with a BC value of <9 mL/cm H2O in the end stage (72%, 73%, vs. 66%), but the SEN, PPV, and NPV were similar (Table 2, Fig. 2). The SEN of a ‚Ė≥Pdet value of >8 cm H2O in the early filling stage, a ‚Ė≥Pdet value of >20 cm H2O in the middle filling stage and a ‚Ė≥Pdet value of >25 cm H2O in the end filling stage were significantly higher than that of a ‚Ė≥Pdet value of >40 cm H2O in the end stage (82%, 85%, 85%, vs. 49%). A ‚Ė≥Pdet value of >20 cm H2O in the middle filling stage was a better predictor of UUTD, with a PPV and NPV of 76% and 89%, respectively, according to the ROC curve (Table 3, Fig. 3). The DLPP of all children showed that a DLPP value of >20 cm H2O showed significance in predicting UUTD (Table 4, Fig. 4).
The detail relationship between bladder dysfunction and UUTD is still unclear and understanding its mechanism has always been an arduous task for urologists. Children with NB are more likely to develop VUR because of the immature mechanism of anti-reflux at the ureterovesical junction [3] or secondary to pathophysiological changes in the lower urinary tract, which contributes to UUTD. Urodynamic parameters are well known objective evidence to evaluate bladder function and it is important to investigate whether they and/or which one could be a more accurate parameter to predict UUTD during grow and mature of children with NB.
Normal micturition involves passive, low pressure bladder filling during the urine storage phase, while voiding requires the coordination of detrusor contraction and relaxation of the internal and external urinary sphincters. However, in pediatric patients with NB, high filling pressure of the bladder is caused by a pathological bladder wall, which can lead to UUTD. In NB, the inhibition of the pontine micturition center is weakened due to damage to the cortical and subcortical structures, which usually results in decreased bladder filling consciousness and low bladder capacity [18]. In addition, the pathophysiological changes in NB show individual variations. Therefore, it is not surprising that the values of low BC vary, ranging from 10 to 40 mL/cm H2O. Kaufman et al. [19] considered a ‚Äė‚Äėbladder storage pressure‚Äô‚Äô of 40 cm H2O at typical filling capacity to be the pressure level for upper tract dilatation.
Two parameters, BC and ‚Ė≥Pdet, have been reported in the literature to predict UUTD, and UUTD can be predicted according to the method by which the ICCS recommends calculating BC, but its accuracy is still not high. An ICS Teaching Module also showed that DLPP should not be used as the sole urodynamic parameter for predicting UUTD [20].
Kurzrock and Polse [4] and Ghoniem et al. [5] observed children with myelomeningocele or spina bifida in urodynamic studies and found that low BC was closely related to UUTD. A meta-analysis also suggested that low BC and high DLPP were major risk factors for UUTD [10]. Our results supported this finding, showing that the BC values of 3 filling stages in UUTD group were smaller than those in the no UUTD group significantly. Low BC could result in higher intravesical pressure than normal bladder and destroy the support of the detrusor muscle at the ureterovesical junction, resulting in the failure of the normal anti-reflux mechanism.
Kurzrock and Polse [4] reported that BC value of <9 mL/cm H2O was a better predictor of UUTD, with a poor PPV (52%). In our study, the PPV of BC value of <9 mL/cm H2O was only 60% and the PPV of BC value of <8 mL/cm H2O in the end filling stage was 65%. Neither were satisfactory for predicting UUTD. Therefore, it is not certain that the new indicator is more accurate than the classical indicator.
In addition, McGuire et al. [1] reported that a ‚Ė≥Pdet value of >40 cm H2O was a risk factor for UUTD, with a PPV of 70%. In our study, the ROC curve revealed that the PPV of a ‚Ė≥Pdet value of >40 cm H2O was 75%, but its SEN was only 49%, which was similar to the study of Teichman et al. [21]. Kurzrock and Polse [4] also indicated that a ‚Ė≥Pdet value of <40 cm H2O can effectively prevent the development of UUTD (according to results after 11 years of follow-up). According to the ICCS definition of pediatric bladder function, a ‚Ė≥Pdet value of ‚ȧ10 cm H2O could be considered essentially normal when the child‚Äôs bladder is filling to the expected capacity. Styles et al. [22] analyzed the relationship between UUTD and BC in 25 patients with chronic urine retention and found that there were statistically significant correlations between UUTD and both a high detrusor pressure in the end filling stage (Pdet >25 cm H2O) and a pressure increase during filling (‚Ė≥Pdet >15 cm H2O). The sensitivity was 93 and 100%, but the specificity was low (64% and 45%). Ozkan et al. [23] analyzed the urodynamic data of 35 patients with NB who did not undergo surgical treatment and found that a DLPP value of >75 cm H2O was a fairly high risk factor for UUTD. However, its PPV was not high (41%). In addition, the study of √áetinel et al. [24] showed similar findings. In our study, a DLPP value of >20 cm H2O showed significance in predicting UUTD but also had a low PPV (50%). Therefore, we know that a low BC, ‚Ė≥Pdet, and high DLPP in the filling period are risk factors for UUTD in children with NB, but the parameters established in the literature are not satisfactory and cannot accurately predict UUTD [4,22,23].
Obviously, the identification of more accurate parameters or methods to predict UUTD is necessary. One method is to measure the value of BC in different filling stages. Early in 1989, Ghoniem et al. [6] divided BC into ‚Äė‚Äėinitial‚Äô‚Äô and ‚Äė‚Äėterminal‚Äô‚Äô stages, when the initial slow rise in bladder pressure may turn into a rapid increase. By comparison, patients with good initial compliance did well clinically, while patients with poor initial compliance more commonly had VUR, deteriorated upper urinary tract morphology, and impaired renal function. He also found that a high DLPP (40 cm H2O or greater) and low BC (less than 10 mL/cm H2O) seem to be strong predictors of children at risk of UUTD [5].
In 1993, Gilmour et al. [25] analyzed the value of BC in different filling stages in 63 normal children and revealed that the minimum BC of normal bladder in normal children is 10 mL/cm H2O. He divided the filling process into 3 stages similar to ours but did not analyze them in detail by numerical values in children with NB. Present study showed detail numerical values of early filling stage, lower BC value is of little significance to UUTD. In this stage, the lower intravesical pressure achieved is due to the bladder is still empty. At the beginning of the middle filling stage, a further increase in bladder volume accompanied by a significant increase in intravesical pressure was observed, it might be due to the rate of stretch exceeds the rate of stress relaxation and then remains balanced as well as BC rises slowly. When the bladder continues to be filled in the end filling stage, the elasticity of the bladder gradually reaches its maximum elastic limit, and the pressure is not changed significantly anymore.
Therefore, we investigated BC in 3 different bladder filling stages and its relationship to UUTD and has found its good predictive value. The P-V curves in the majority (80%) of the patients with NB in our study showed a special characteristic; therefore, we divided the filling process into 3 stages. The first stage (early filling stage) showed that the detrusor pressure increased slowly, the second stage (middle filling stage) revealed that the detrusor pressure increased quickly and then continued to increase slowly, and the end stage (end filling stage) showed that the detrusor pressure was at a stably high level. This observation may be related to the increased stiffness caused by bladder fibrosis in children with NB. This phenomenon suggests that the ‚Ė≥Pdet value in different filling stages could predict UUTD more accurately. Our study showed that a BC value of <10 mL/cm H2O was found in 76% of patients with NB in different filling stages. The accuracy of a BC value of <8 mL/cm H2O in the middle and end filling stages in predicting UUTD was slightly higher than that of a BC value of <9 mL/cm H2O, and a ‚Ė≥Pdet value of >20 cm H2O in the middle filling stage had high accuracy, with an SEN of 85%, which was significantly higher than that of a ‚Ė≥Pdet value of >40 cm H2O. The PPVs were similar (76% vs. 75%). The ability of a ‚Ė≥Pdet value of >8 cm H2O to predict UUTD in the early filling stage was limited because its PPV was only 67%, which was lower than that of the study of McGuire et al. [1]. It is obvious that a ‚Ė≥Pdet value of >20 cm H2O in the middle filling stage is a better predictor of UUTD. Overall, the ability of BC and ‚Ė≥Pdet to predict UUTD in different filling stages is more accurate than reported in the above studies. This provided a possibility of finding an accurate time to perform intermittent catheterization to timely empty the bladder to prevent UUTD [26].
The relationships between other indicators, such as sex, disease course, urinary tract infection, bladder wall thickness, fecal incontinence, and UUTD, need to be further studied [2,7]. Research on the relationship between bladder capacity and UUTD is limited [19]. Çetinel et al. [24] reported that bladder capacity <200 mL was an independent risk factor for patients with spinal cord injury.
The main limitation of this study is that it is difficult to obtain accurate predictions with a small number of patients; the results of this retrospective study therefore need further verification. However, the findings of this study may provide new ideas for prospective studies with larger sample sizes in the future.
In conclusion, a low BC, a high detrusor pressure and an increased DLPP are good urodynamic parameters to predict UUTD, and these parameters reciprocally increase with the development of UUTD in children with NB. Both a ‚Ė≥Pdet value of >20 cm H2O in the middle stage and of 25 cm H2O in the end filling stage are accurate indicators for predicting UUTD, with high sensitivity and specificity.
NOTES
Research Ethics
This study was approved by the Ethics Committee of First Affiliated Hospital of Zhengzhou University (2020-KY-191).
Fund/Grant Support
This study was supported by Henan Province Medical Science Provincial-ministerial Construction Project (No. SBGJ2018059) and National Nature Science Foundation of China (No. U1904208,81670689).
AUTHOR CONTRIBUTION STATEMENT
‚ÄĘ Conceptualization: LL, JGW
‚ÄĘ Data curation: LL, YXY, EPL, YPZ, HJH
‚ÄĘ Formal analysis: LL, FPJ, QSP, XHY
‚ÄĘ Funding acquisition: JGW
‚ÄĘ Methodology: QWW, YW
‚ÄĘ Project administration: JGW
‚ÄĘ Visualization: LL
‚ÄĘ Writing-original draft: LL, YXY
‚ÄĘ Writing-review & editing: QWW, YW, JGW
REFERENCES
1. McGuire EJ, Woodside JR, Borden TA. Upper urinary tract deterioration in patients with myelodysplasia and detrusor hypertonia: a followup study. J Urol 1983;129:823-6. PMID: 6842712


2. Wang W, Fang H, Xie P, Cao Q, He L, Cai W. Create a predictive model for neurogenic bladder patients: upper urinary tract damage predictive nomogram. Int J Neurosci 2019;129:1240-6. PMID: 31401918


3. Wang QW, Wen JG, Song DK, Su J, Che YY, Zhang P, et al. Is it possible to use urodynamic variables to predict upper urinary tract dilatation in children with neurogenic bladder-sphincter dysfunction? BJU Int 2006;98:1295-300. PMID: 17034510


4. Kurzrock EA, Polse S. Renal deterioration in myelodysplastic children: urodynamic evaluation and clinical correlates. J Urol 1998;159:1657-61. PMID: 9554387


5. Ghoniem GM, Roach MB, Lewis VH, Harmon EP. The value of leak pressure and bladder compliance in the urodynamic evaluation of meningomyelocele patients. J Urol 1990;144:1440-2. PMID: 2231938


6. Ghoniem GM, Bloom DA, McGuire EJ, Stewart KL. Bladder compliance in meningomyelocele children. J Urol 1989;141:1404-6. PMID: 2724439


7. Prakash R, Puri A, Anand R, Jain AK, Lal B, Garg V. Predictors of upper tract damage in pediatric neurogenic bladder. J Pediatr Urol 2017;13:503.e1-503.e7. PMID: 28385450


8. Tarcan T, Sekerci CA, Akbal C, Tinay I, Tanidir Y, Sahan A, et al. Is 40cmH2O detrusor leak point pressure cut-off reliable for upper urinary tract protection in children with myelodysplasia? Neurourol Urodyn 2017;36:759-63. PMID: 27080436



9. Wen JG, Yeung CK, Chu WC, Shit FK, Metreweli C. Video cystometry in young infants with renal dilation or a history of urinary tract infection. Urol Res 2001;29:249-55. PMID: 11585280


10. Musco S, Padilla-Fern√°ndez B, Del Popolo G, Bonifazi M, Blok BFM, Groen J, et al. Value of urodynamic findings in predicting upper urinary tract damage in neuro-urological patients: a systematic review. Neurourol Urodyn 2018;37:1522-40. PMID: 29392753


11. Austin PF, Bauer SB, Bower W, Chase J, Franco I, Hoebeke P, et al. The standardization of terminology of lower urinary tract function in children and adolescents: update report from the standardization committee of the International Children’s Continence Society. Neurourol Urodyn 2016;35:471-81. PMID: 25772695


12. Wen JG, Djurhuus JC, Rosier PFWM, Bauer SB. ICS educational module: pressure flow study in children. Neurourol Urodyn 2018;37:2311-4. PMID: 29931789


13. Wen JG, Djurhuus JC, Rosier PFWM, Bauer SB. ICS educational module: cystometry in children. Neurourol Urodyn 2018;37:2306-10. PMID: 30203421


14. Schäfer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 2002;21:261-74. PMID: 11948720


15. Kaefer M, Zurakowski D, Bauer SB, Retik AB, Peters CA, Atala A, et al. Estimating normal bladder capacity in children. J Urol 1997;158:2261-4. PMID: 9366371


16. Hernandez RD, Hurwitz RS, Foote JE, Zimmern PE, Leach GE. Nonsurgical management of threatened upper urinary tracts and incontinence in children with myelomeningocele. J Urol 1994;152(5 Pt 1):1582-5. PMID: 7933209


17. Kaefer M, Pabby A, Kelly M, Darbey M, Bauer SB. Improved bladder function after prophylactic treatment of the high risk neurogenic bladder in newborns with myelomentingocele. J Urol 1999;162(3 Pt 2):1068-71. PMID: 10458433

19. Kaufman AM, Ritchey ML, Roberts AC, Rudy DC, McGuire EJ. Decreased bladder compliance in patients with myelomeningocele treated with radiological observation. J Urol 1996;156:2031-3. PMID: 8965337


20. Tarcan T, Demirkesen O, Plata M, Castro-Diaz D. ICS teaching module: detrusor leak point pressures in patients with relevant neurological abnormalities. Neurourol Urodyn 2017;36:259-62. PMID: 26693834


21. Teichman JM, Scherz HC, Kim KD, Cho DH, Packer MG, Kaplan GW. An alternative approach to myelodysplasia management: aggressive observation and prompt intervention. J Urol 1994;152(2 Pt 2):807-11. PMID: 8022020


22. Styles RA, Ramsden PD, Neal DE. Chronic retention of urine. the relationship between upper tract dilatation and bladder pressure. Br J Urol 1986;58:647-51. PMID: 3801823


23. Ozkan B, Demirkesen O, Durak H, Uygun N, Ismailoglu V, Cetinel B. Which factors predict upper urinary tract deterioration in overactive neurogenic bladder dysfunction? Urology 2005;66:99-104. PMID: 15992868


24. √áetinel B, √Ėnal B, Can G, Talat Z, Erhan B, G√ľnd√ľz B. Risk factors predicting upper urinary tract deterioration in patients with spinal cord injury: a retrospective study. Neurourol Urodyn 2017;36:653-8. PMID: 26934371


25. Gilmour RF, Churchill BM, Steckler RE, Houle AM, Khoury AE, McLorie GA. A new technique for dynamic analysis of bladder compliance. J Urol 1993;150:1200-3. PMID: 8371391


26. Wang QW, Song DK, Zhang XP, Wu YD, Zhang RL, Wei JX, et al. Urodynamic parameters development and complications of clean intermittent self-catheterization in Chinese schoolchildren with neurogenic underactive bladder. Urol Int 2011;86:461-5. PMID: 21555862


Fig. 1.
A female with upper urinary tract dilatation, 14 years old, 7 years after spinal cord trauma operation. Bladder compliance decreased significantly (bladder compliance <5 mL/cm H2O). In the middle filling stage, the detrusor pressure increased quickly (red arrow) and then slowly
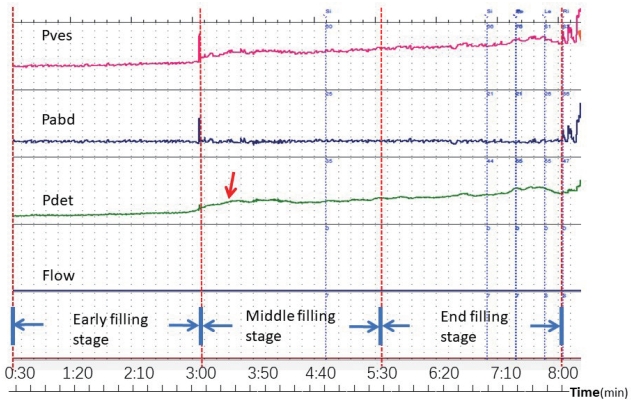
Fig. 2.
Receiver operating characteristic curve of bladder compliance (BC) in different filling stages predicting upper urinary tract dilatation. The cutoff value of BC2 is 8.21 (AUC=0.797). The cutoff value of BC3 is 8.24 (AUC=0.785). AUC, area under the curve.
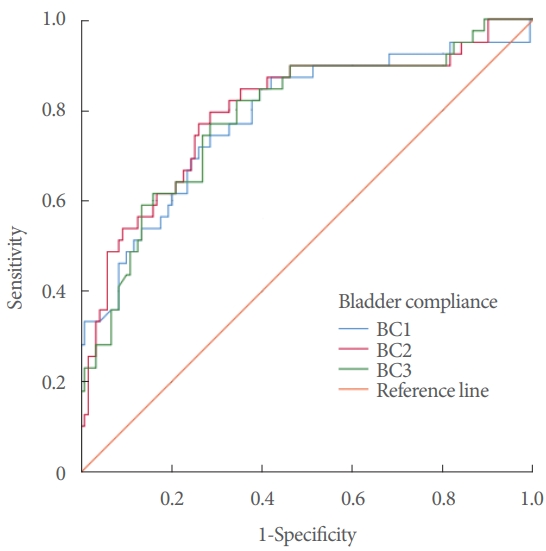
Fig. 3.
Receiver operating characteristic curve of ‚Ė≥Pdet in different filling stages predicting upper urinary tract dilatation. The cutoff value of Pdet1 is 7.7 (AUC=0.810). The cutoff value of ‚Ė≥Pdet2 is 19.5 (AUC=0.845). The cutoff value of ‚Ė≥Pdet3 is 24.5 (AUC=0.816). ‚Ė≥Pdet, detrusor pressure; AUC, area under the curve.

Fig. 4.
Receiver operating characteristic curve of the detrusor leak point pressure (DLPP) in all patients predicting upper urinary tract dilatation. The cutoff value of DLPP is 19.5 (AUC=0.657). AUC, area under the curve.
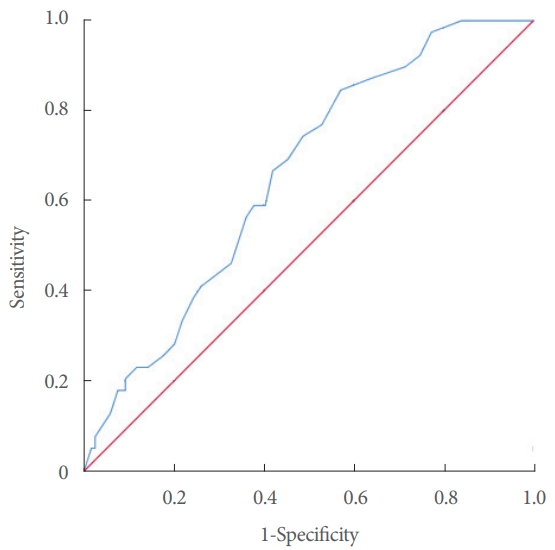
Table 1.
Characteristics of patients with neurogenic bladder
| Characteristic | UUTD group (n = 39) | Control group (n = 119) | t (Ōá2) | P-value |
|---|---|---|---|---|
| Sex (male:female) | 21:18 | 68:51 | 0.030 (Ōá2) | 0.862 |
| Age (yr) | 8.5 ¬Ī 2.9 | 7.9 ¬Ī 4.5 | 0.780 | 0.437 |
| Disease | 0.041 (Ōá2) | 0.839 | ||
| ‚ÄÉSpina biÔ¨Āda | 30 | 93 | ||
| ‚ÄÉCystic spina biÔ¨Āda repaired | 6 | 18 | ||
| ‚ÄÉSpina bifida injury | 3 | 8 | ||
| BC (mL/cm H2O) | ||||
| ‚ÄÉEarly filling stage (BC1) | 13.17 ¬Ī 26.71 | 21.37 ¬Ī 23.31 | 1.838 | 0.068 |
| ‚ÄÉMiddle filling stage (BC2) | 9.49 ¬Ī 13.22 | 28.66 ¬Ī 35.68 | 3.277 | 0.001* |
| ‚ÄÉEnd filling stage (BC3) | 9.88 ¬Ī 12.97 | 30.08 ¬Ī 43.75 | 2.837 | 0.005* |
| ‚Ė≥Pdet (cm H2O) | ||||
| ‚ÄÉEarly filling stage (‚Ė≥Pdet1) | 15.59 ¬Ī 10.06 | 5.91 ¬Ī 4.74 | 8.134 | 0.00* |
| ‚ÄÉMiddle filling stage (‚Ė≥Pdet2) | 27.48 ¬Ī 12.2 | 11.64 ¬Ī 9.12 | 8.621 | 0.00* |
| ‚ÄÉEnd filling stage (‚Ė≥Pdet3 | 37.09 ¬Ī 15.96 | 17.8 ¬Ī 13.97 | 7.218 | 0.00* |
| DLPP (cm H2O) | 28.9 ¬Ī 9.27 | 23.98 ¬Ī 9.46 | 2.830 | 0.005* |
Table 2.
The accuracy of BC in different filling stages predicting UUTD
|
In the middle filling stage |
In the end filling stage |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| BC (mL/cm H2O) | SEN (%) | SPE (%) | PPV (%) | NPV (%) | BC (mL/cm H2O) | SEN (%) | SPE (%) | PPV (%) | NPV (%) |
| <4 | 36 | 94 | 80 | 69 | <4 | 28 | 95 | 79 | 66 |
| <6 | 56 | 85 | 71 | 74 | <6 | 56 | 87 | 74 | 75 |
| < 8a) | 77 | 72 | 65 | 82 | < 8a) | 74 | 73 | 65 | 81 |
| <9 | 82 | 67 | 62 | 85 | <9 | 77 | 66 | 60 | 81 |
| < 10 | 85 | 63 | 61 | 86 | < 10 | 82 | 64 | 60 | 84 |
| < 12 | 85 | 60 | 59 | 86 | < 12 | 85 | 59 | 58 | 86 |
| < 14 | 87 | 56 | 57 | 87 | < 14 | 87 | 55 | 56 | 86 |
| < 16 | 87 | 54 | 56 | 86 | < 16 | 90 | 50 | 55 | 88 |
Table 3.
The accuracy of ‚Ė≥Pdet in different filling stages predicting UUTD
|
In the early filling stage |
In the middle filling stage |
In the end filling stage |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ‚Ė≥Pdet (cmH2O) | SEN (%) | SPE (%) | PPV (%) | NPV (%) | ‚Ė≥Pdet (cmH2O) | SEN (%) | SPE (%) | PPV (%) | NPV (%) | ‚Ė≥Pdet (cmH2O) | SEN (%) | SPE (%) | PPV (%) | NPV (%) |
| > 20 | 23 | 99 | 94 | 66 | > 40 | 10 | 98 | 77 | 62 | > 40 | 49 | 89 | 75 | 72 |
| > 15 | 51 | 94 | 85 | 74 | > 35 | 28 | 97 | 86 | 67 | > 35 | 59 | 84 | 71 | 75 |
| > 10 | 67 | 84 | 74 | 79 | > 30 | 39 | 94 | 81 | 70 | > 30 | 67 | 81 | 70 | 79 |
| > 8a) | 82 | 73 | 67 | 86 | > 25 | 58 | 89 | 78 | 76 | > 25a) | 85 | 77 | 71 | 89 |
| >6 | 85 | 60 | 59 | 86 | > 23 | 72 | 87 | 79 | 82 | > 23 | 87 | 73 | 68 | 89 |
| >4 | 87 | 52 | 55 | 86 | > 20a) | 85 | 82 | 76 | 89 | > 20 | 90 | 65 | 63 | 91 |
| - | - | - | - | - | > 18 | 87 | 77 | 72 | 90 | > 18 | 90 | 64 | 63 | 91 |
| - | - | - | - | - | > 16 | 90 | 74 | 70 | 92 | > 16 | 90 | 59 | 59 | 90 |
Table 4.
The accuracy of DLPP in all patients predicting UUTD
| DLPP (cm H2O) | SEN (%) | SPE (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|
| > 40 | 18 | 92 | 60 | 63 |
| > 35 | 26 | 82 | 49 | 62 |
| > 30 | 44 | 71 | 50 | 66 |
| > 25 | 59 | 60 | 50 | 69 |
| > 20a) | 85 | 43 | 50 | 81 |
| > 15 | 97 | 23 | 46 | 92 |
| > 10 | 100 | 100 | 100 | 100 |





