Is the Reference Electrode Location Important for the Electromyography Evaluation of the Pelvic Floor in Urodynamic Studies?
Article information
Abstract
Purpose
Perineal electromyography (EMG) is a crucial part of urodynamic studies. Many researchers focused on the standardization of techniques in urodynamics, but no study has yet evaluated the differences with various reference electrode placements. The aim of this study was to determine the optimal placement of the reference electrode for recording pelvic floor activity in urodynamic studies.
Methods
Children over 6 years of age without anatomic or neurological abnormalities were invited to participate in the study. Four reference electrodes were placed on the right kneecap, the inner surface of the right inner thigh, the right anterior iliac spine (AIS), and the skin over the left gluteal muscles for simultaneous recording. The EMG signal formed by pelvic contraction during forceful straining was recorded both in the supine and sitting positions. The root mean square (RMS) value of each muscle contraction signal was calculated.
Results
Twenty-one participants (10 boys and 11 girls) were included. The mean age was 10.19±3.20 years. The highest RMS values were obtained with the reference electrode on the thigh in the supine position and the AIS in the sitting position. Significant differences were found between the mean RMS values of the knee and other locations of reference electrodes in the supine position, as well as between mean RMS values in all regions except the thigh and gluteus in the sitting position. The minimum mean RMS values in both positions were obtained with the reference electrode on the knee.
Conclusions
During urodynamic studies, reference electrodes shall be placed on AIS in the sitting and on the inner thigh in the supine position. The knee is not a suitable option for reference electrode placement. This information may help improve EMG recordings in the evaluation of pelvic floor muscles.
INTRODUCTION
Electromyography (EMG) is a diagnostic method to evaluate the muscles and motor neurons [1]. At least 3 electrodes are used to record surface EMG. The potential difference between the 2 active electrodes is amplified and brought to an observable level. A reference electrode is needed to measure the value of this difference based on a reference value.
Perineal EMG is a crucial part of urodynamic studies. A reference electrode is needed when evaluating pelvic floor activity [2]. Many researchers have focused on the standardization of techniques in urodynamic studies [3-5]. Proper placement of the surface electrodes is essential for obtaining an appropriate EMG recording. However, the placement of the reference electrode has not received enough attention. Traditionally, it is placed on the inner thigh [2,5,6]. However, Siroky recommended placing the reference electrode on bone without muscle activity, such as the anterior part of the iliac bone [7]. To our knowledge, no study in the literature has compared possible reference points. We speculated that differences in reference electrode placement might affect the results of EMG recordings during pelvic floor evaluation. We planned a study to determine the optimal placement of the reference electrode for recording pelvic floor activity in urodynamic studies.
MATERIALS AND METHODS
Study Group
Patients over 6 years of age who were scheduled for uroflowmetry in our department with no anatomical or neurological abnormalities were invited to participate in our study. After consent, children were informed about anal sphincter and pelvic floor activity. They were then instructed to tighten their anus in the supine frog-leg position. Patients who had abnormal EMG findings and those who could not perform this maneuver were excluded from the study. This study was approved by the local ethics committee of the Ege University Faculty of Medicine (19- 11.1T/47). The optimization of EMG recordings is particularly essential in pediatric practice; therefore, this study was performed in children. The study was conducted according to the criteria set by the Declaration of Helsinki, and each subject and parent signed informed consent before participating in the study.
Measurement Setup
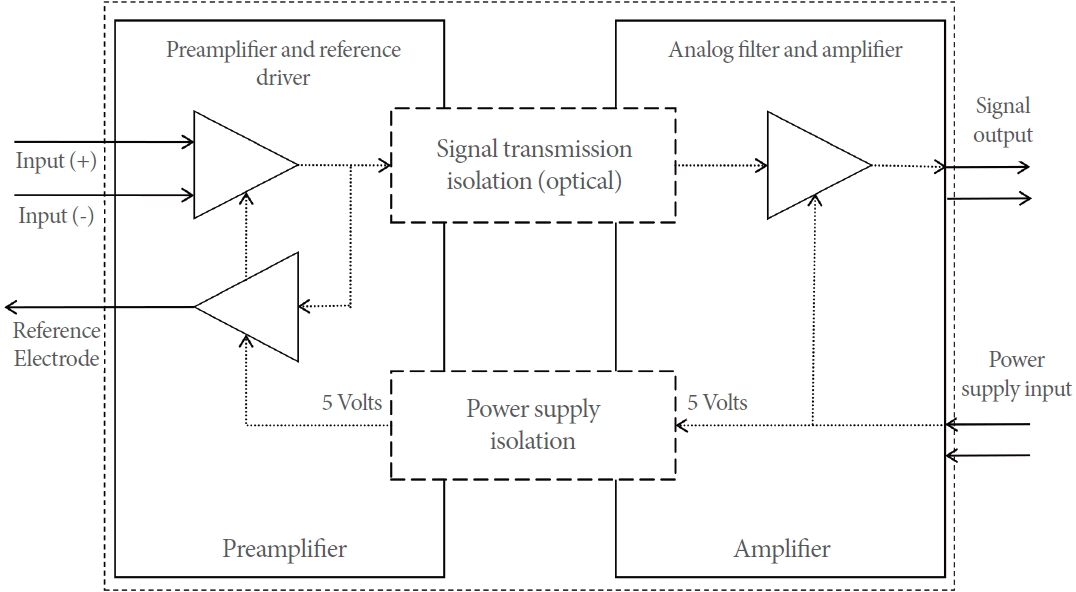
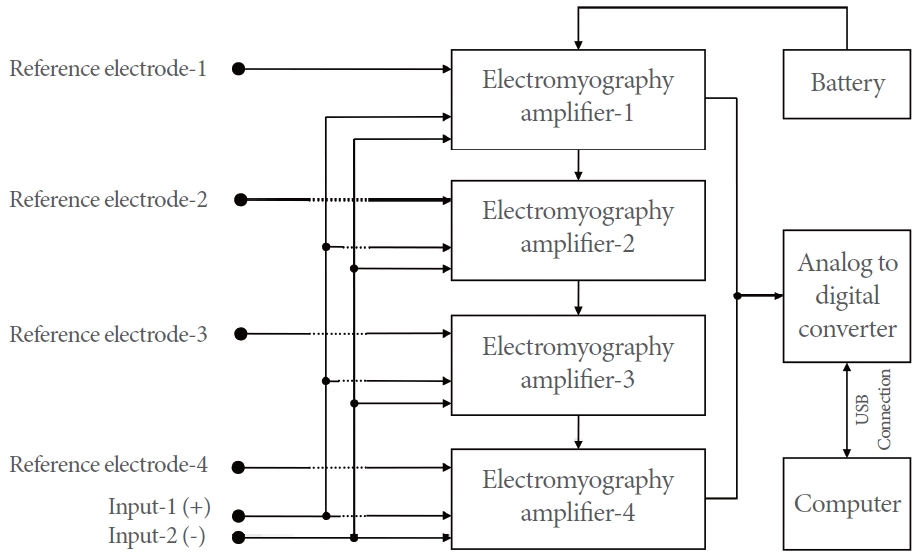
Four identical EMG amplifier modules (Aymed Medical Tech, Istanbul, Turkey) with electrically isolated inputs (Fig. 1), one 10,000-mAh capacity battery unit (power bank-model no: DLP6710CV; Philips, Amsterdam, The Netherlands), an analog-to-digital converter module with inputs at a 50 kHz sampling rate per channel with 16-bit resolution (USB-1808X, Measurement Computing Corp., Norton, MA, USA), DASYLab software, (Data Acquisition System Laboratory, measX GmbH & Co. KG, Moenchengladbach, Germany), and a recording program prepared with this software were used to record on a portable computer. A schematic diagram of the measurement setup is given in Fig. 2.
A common input was constituted by connecting the negative and positive inputs of each EMG amplifier. Reference electrodes were placed on different locations connected to EMG amplifiers independently. All hardware except the computer was housed in a box with a large metal plate on the base. The negative terminals of the battery and the analog-digital converter were connected to this metal plate to reduce the environmental noise.
Biopotential Amplifier and Analog-to-Digital Converter Module Calibration
All amplifiers and the inputs of the analog-to-digital converter module were made of exactly the same parts or materials, but there may still have been some minor differences. Signals with a known amplitude or potential difference were applied to the inputs of these modules by means of a signal generator in order to overcome this issue. Then, their outputs were measured by means of an oscilloscope and a voltmeter. Calculations were made to assess whether the analog-to-digital converter performed linear digitization. Equations with necessary corrections for existing minor differences were defined in the recording and analysis software.
Analog-Digital Conversion and Data Recording Software
The signals received from the EMG amplifiers were connected to 4 inputs of the analog-digital converter module, which could run each channel with 16-bit resolution simultaneously and independently. The analog-to-digital conversion module sent the incoming signal to the computer at a rate of 50,000 samples per second. DASYLab software was used as a recording and analysis program. In this software, modules as figures representing certain functions are connected to each other with lines, and then a running program is created. A depiction of the structured program is given in Fig. 3.
Analysis of the Records
The root mean square (RMS) is a statistical parameter used to measure the magnitude of varying quantities. It is especially useful in waves where the change is positive and negative. It is defined as the square root of the mean square (the arithmetic mean of the squares of a set of numbers). It represents the magnitude of a waveform in the time axis. The data were analyzed with software prepared with modules in the DASYlab program. The RMS value of each muscle contraction signal was calculated.
EMG Recording Method
After skin preparation with an alcohol-based solution, self-adhesive gel skin electrodes (Aymed, Istanbul, Turkey) were placed on the right and left sides near the anus in the supine frog-leg position. These electrodes were connected to the recording device as active electrodes.
The first electrode to be used as a reference was placed on the skin on the right kneecap, the second on the skin on the inner surface of the right inner thigh, the third on the right anterior iliac spine (AIS) skin, and the fourth on the skin over the left gluteal muscles (Fig. 4).
All subjects were taught how to contract the pelvic floor muscles before the recording and were asked to perform one or 2 short-term contraction exercises. During the recording, the subjects were instructed to contract their pelvic floor muscles as strong and long as they could. The EMG signal formed by pelvic contraction was recorded. The recordings were performed twice, in the supine position on the examination table and the sitting position on the urodynamic chair.
Statistical Analysis
The data were analyzed using IBM SPSS Statistics ver. 23.0 (IBM Co., Armonk, NY, USA). The normality of the data distribution was assessed with the Kolmogorov-Smirnov test. Nonparametric values were analyzed with the Wilcoxon test and parametric values with the t-test. A P-value less than 0.05 was defined as statistically significant.
RESULTS
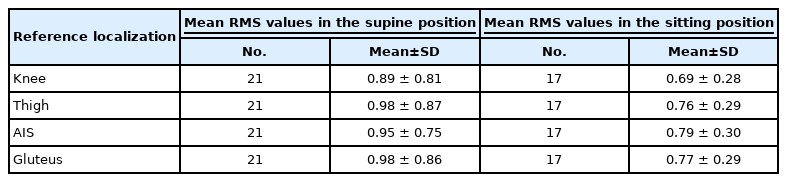
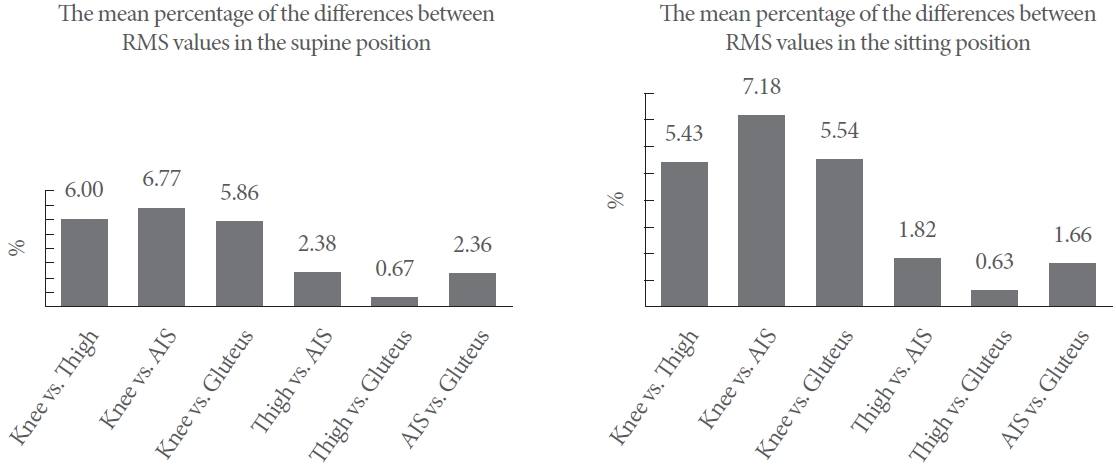
In total, 21 subjects (10 boys and 11 girls) were included in the study. The mean age was 10.19±3.20 years. The RMS values could not be recorded in the sitting position in 5 patients due to a lack of cooperation. The mean RMS values at the supine and sitting positions are given in Table 1. The highest RMS values were obtained with the reference electrode on the thigh in the supine position and the AIS in the sitting position. Significant differences were found between the mean RMS values of the knee and other locations of reference electrodes in the supine position. There were also significant differences between the mean RMS values in all regions except the thigh and gluteus in the sitting position. The minimum mean RMS values in both positions were obtained with the reference electrode on the knee. The statistical significance of the mean RMS values according to the reference localizations is given in Table 2.
The mean percentages of the differences between each channel were calculated (Fig. 5). The knee and AIS electrodes had the most divergent values. P-values for the differences between RMS values of the 2 compared regions are given in Table 2.
DISCUSSION
Many studies have investigated the techniques of EMG examinations; however, few studies have described the reference electrode location [6-10]. There are currently no scientific data providing a rationale for the choice of reference electrode location. This study aimed to find solid evidence for the proper placement of the reference electrode.
EMG is an integral part of urodynamic studies. Disposable surface electrodes have been widely used for many years [5,6]. The optimum performance of EMG depends on the correct placement of the electrodes [11]. The location of active electrodes in EMG is determined simply and precisely by the location of the target muscle, with the aim of being close as possible. However, there is no evidence for the optimal location of the reference electrode. Barrett used the thigh as the reference electrode site, which was followed by other researchers [6]. Our study showed that this location, with the highest RMS value in the supine position, is a reasonable suggestion.
Bony prominences, hypothetically being electrically unaffected areas, have also been suggested as a better option for placing reference electrodes [8]. Therefore, Siroky recommended the AIS [7]. We also included the kneecap in our study as an alternative bony prominence. Our results suggested that the AIS was the third-best option in the supine position but the best option in the sitting position. This may be related to positional involuntary contractions of the thigh and gluteal muscles. This undesired muscle activity in the reference electrode can decrease the RMS value; thus, it interferes with the studied pelvic floor muscle. The knee had the lowest mean RMS value. The probable reason for this result was the longer distance from active electrodes and signal interference caused by this distance.
Although a urodynamic examination in a sitting position gives better results, supine urodynamics may be more ergonomic in patients with mobility impairments. Therefore, we evaluated the performance of EMG electrodes in different patient positions. Our study showed that the difference between different positions for each electrode was small.
The reliability of EMG studies is frequently questioned due to the lack of standardization in many aspects [12]. Well-designed studies are required to standardize techniques in urodynamics. Performed with the motivation of contributing to this goal, our study revealed that the AIS and thigh were the most suitable locations to place the reference electrode in urodynamic studies. The knee proved to be a less suitable location for reference electrode placement.
The record system setup was specifically designed with the following features to investigate the effects of the reference electrode position: Measurements from all locations with 4 identical EMG amplifiers through 4 simultaneous analog-to-digital conversion processes made it possible to analyze the same EMG signal in real time without any difference at the inputs except the reference electrode. The EMG amplifiers with electrically isolated inputs (Fig. 1) allowed us to combine the inputs into a common input and made it possible to place the reference input of each amplifier at a different location without any electrical interference. Otherwise, any other EMG amplifier without an isolated input would electrically interfere with each other if set up as in Fig. 2. Placing a large metal plate (~25 ×25 cm) connected to the negative terminal power supply of the recording box and powering the entire system with batteries including the computer and EMG amplifiers with a high common mode rejection ratio of ~110 dB made it possible to record extremely clean signals without any interference or noise to achieve reliable results. Finally, each amplification and analog-to-digital conversion channel was calibrated using external signal sources for possible minor differences or errors in the amplification and conversion slope, and these errors were corrected in the recording software for perfect similarity. The steps enabled a reliable comparison of the signals recorded. We also repeated the study in both supine and sitting positions in order to analyze positional variations.
There are some limitations of this study. The results may not reflect clinically substantial differences since the RMS values were very similar. Placing a reference electrode on the skin over the gluteus may not affect the EMG results.
In conclusion, our study revealed that different options for reference electrode placement result in slight differences between EMG recordings. The knee is not a suitable option for placing the reference electrode. The AIS should be the preferred location for the reference electrode in the sitting position and the inner thigh in supine position during urodynamic studies. This information may help improve EMG recordings in the evaluation of pelvic floor muscles.
Notes
Funding/Grant Support
This study was supported by Ege University Scientific Research Projects Coordination Unit.
Research Ethics
This study was approved by the local ethic committee of the Ege University Faculty of Medicine (19-11.1T/47).
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION STATEMENT
·Conceptualization: AT, MP, IZA, IU
·Data curation: AT, OBY, UB, HÇ, IZA
·Formal analysis: MP, ST, HÇ, IU
·Methodology: AT, MP, IU
·Writing - original draft: AT, ST, OBY, UB, IU
·Writing - review & editing: MP, ST, HÇ, IZA, IU