Water Vapor Therapy and Zonal Anatomy of the Prostate
Article information
Abstract
Water vapor therapy using Rezūm has been recently introduced as a minimally invasive surgery for benign prostatic hyperplasia and is being increasingly performed. However, there is a lack of real-time images showing this practice and how convective water vapor acts in the prostate gland. In real-time ultrasonography, convective water vapor rapidly spreads throughout the ipsilateral transitional zone and is mostly limited within the transitional zone. For educational purposes, we would like to present a case to help readers understand water vapor therapy by visualizing convective water vapor using real-time ultrasound.
Although the first paper for Rezum was reported in 2015, there is no real-time image of how the convective water vapor acts in the prostate gland. Very recently, on June 27, 2023, the first water vapor therapy was performed in South Korea. We thought that the visualization using real-time ultrasound during the water vapor therapy could inspire surgeons who wonder how the mechanism really works. We provide here a short video clip and relevant explanations showing real-time ultrasound of convective water vapor during water vapor therapy using Rezum.
CASE REPORT
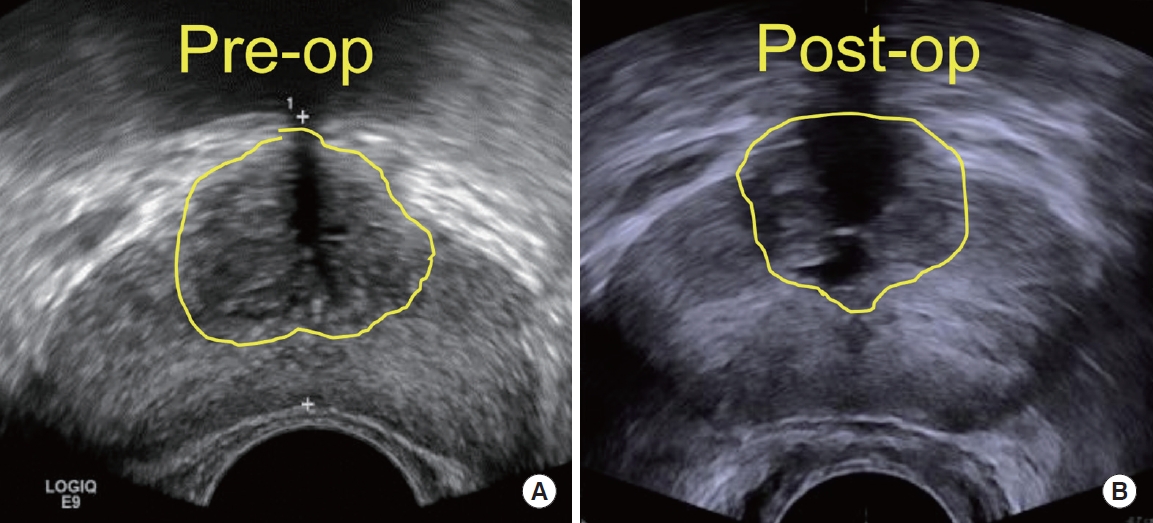
A 62-year-old man who was sexually active presented with acute urinary retention. Catheterization and the administration of an alpha-1 antagonist for 3 days facilitated him in voiding by himself. After a month, the patient visited the outpatient clinic to evaluate voiding function. Serum prostate-specific antigen level (ng/mL), prostate size (total/transitional, mL), International Prostate Symptom Score (IPSS) score, maximum urine flow rate (Qmax; mL/sec), and International Index of Erectile Function (IIEF-5) score were 1.10, 40.2/8.6, 15, 9.8, and 15, respectively. He wanted to undergo prostate surgery and desired to maintain his ejaculatory function. We had no choice but to perform water vapor therapy (WVT). During the operation, it was enough for us to deploy the vapor needle into only 2 points (each point at 8 and 4 o’clock on the lateral lobes). At 3 months after the operation, the prostate-specific antigen level (ng/mL), prostate size (total/transitional, mL), IPSS score, Qmax (mL/ sec), and IIEF-5 score were 1.06, 34.1/5.6, 5, 15.1, and 14, respectively. The reduction volumes of the total prostate and transitional zone were 15.2% and 34.8%, respectively, in the present study (Fig. 1). There were no postoperative complications.
DISCUSSION
According to McVary et al. [1], WVT for benign prostatic hyperplasia (BPH) improved urinary symptoms and the Qmax by approximately 50%, which was maintained over 5 years [1]. Considering that transitional zone growth is the main contributor to BPH progression [2], BPH procedures including WVT should make a therapeutic effect on the transitional zone of the prostate. Now that there was a report indicating that specimens had defects around the prostatic urethra after WVT, which was identified by vital staining [3], we could assume that convective vapor mainly acts in the transitional zone of the prostate. Wong et al. [4] showed that the prostatic urethra was wider than the baseline size in postoperative cystoscopy. However, there has been a lack of real-time images showing WVT, so surgeons may wonder how convective water vapor spreads into the prostate, or surgeons might have a concern for unrecognized complications such as adjacent organ damage. Therefore, visualization of vapor convection may offer readers comprehensive information for the range of convection when WVT is performed.
It was not comfortable for us to apply ultrasound simultaneously during WVT because we had to manipulate a delivery device that was attached to a cystoscope. In fact, surgeons do not have to use intraoperative ultrasonography during WVT. However, by watching a short video clip that we provided, physicians may recognize the approximative boundary of water vapor in the transitional zone and may understand why we keep the injection point 1 cm (approximately 2 fields of view) away from the bladder neck and other injection points [5]. Convective water vapor spreads rapidly to approximately 1 cm from the deployment site and was mostly limited to the transitional zone (Supplementary video clip); however, tiny streams seemed to be delivered into the ipsilateral peripheral zone.
SUPPLEMENTARY MATERIALS
Supplementary Video clip can be found via https://doi.org/inj.2346278.139.
Notes
Research Ethics
The Institutional Review Board of St. Vincent’s Hospital approved this case study design and access to the patients’ medical records (approval number: VC23ZASI0165, approval date: July 14, 2023). This study was performed in accordance with the Declaration of Helsinki. This article does not reference any animal studies performed by any of the authors. Informed consent was obtained from the participant in the study.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTION STATEMENT
· Conceptualization: JHK, DSL
· Data curation: HYK
· Methodology: HYK
· Project administration: SJL
· Writing - original draft: DSL
· Writing - review & editing: JHK